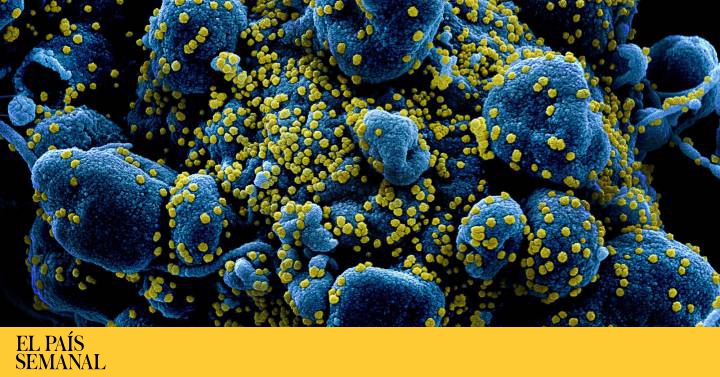
Virologist Luis Enjuanes has been studying coronaviruses for 35 years. It works with pathogens such as the one that causes severe acute respiratory syndrome (SARS CoV-1) or MERS-CoV, the deadliest, which kills one in three people. At the end of March, he was counting on the other end of the phone that he had tested positive for SARS-CoV-2, the new coronavirus that has the world on edge. "We have been working in high biological security laboratories for 17 years and we have never been infected." The contagion should have come from outside his laboratory at the CSIC's National Center for Biotechnology (CNB), but it has not been confirmed. His team has reconstructed non-infectious versions of the coronavirus there with genetic engineering techniques. And now they represent one of the most powerful hopes for a highly effective Spanish vaccine against this virus.
When word came of a mysterious pneumonia in China late last year, Enjuanes was directing a doctoral thesis on MERS-CoV, the virus that jumped into humans from dromedaries years ago, although it turned out to be poorly spread between people. His laboratory had developed a vaccine that, tested in humanized mice, conferred 100% protection against the killer, but no one was interested in a vaccine for people. "The companies did not have an excessive interest in it then and we did not come to a development to test it, it is a little frustrating," he laments now. Despite this, research and technology obtained in times of political indolence and the usual shortage of funds for Spanish science have now become pure gold due to a pandemic that has confined half humanity to their homes. Enjuanes confesses that he has never seen politicians react so quickly to drop money to accelerate investigations. It is an old tale; Powers turn to science in times of crisis, but will be forgotten when order is restored.
Instead, Chinese scientists did rush to release the genetic sequence of Wuhan's new CoV-2 virus last January. Enjuanes compared this genetic portrait to that of the SARS virus, which appeared in 2002 causing great alarm. "At first I thought this new coronavirus would go its own way."
And as can happen to even the most expert, the biology of the new virus played a trick.
Although it takes a few more months, the immune response that our vaccine will induce may be higher than that of other vaccines "
The virologist Luis Enjuanes. / ALFREDO CÁLIZ
SARS CoV-1 caused pneumonia that killed 1 in 10 infected people. “It came in the month of November 2002, but they didn't realize it. Alerts in Hong Kong jumped in January. And in April the last case was detected. ” The virus had a total journey of seven months, after massive test campaigns, cancellation of flights to Asia, control of passengers at airports and localized quarantines. In June 2003, it was officially isolated and neutralized. Unfortunately, the Wuhan coronavirus has not followed this path.
"I soon realized that this virus had special characteristics, a personality of its own," continues Enjuanes. “And the worst of all was that he didn't give himself away. It remained hidden for a long time. That upset all the investigations. When they tried to find its origin, the virus was already very widespread. "
Viruses follow the maxim of surviving, infecting the more the better. There is a well-known evolutionary rule among virologists: when a virus spreads it produces variants, but those are selected that are the most attenuated and usually lose virulence. "If a virus is very deadly, you immediately go to the hospital, they quarantine you or bury you, but that virus no longer circulates."
The attenuated forms usually win the battle over the aggressive ones. But Wuhan's coronavirus haggled over to experts. A person without symptoms but infected had a viral load similar to another patient: someone asymptomatic and healthy spreads the virus as easily as someone who coughs. Enjuanes does not remember seeing anything like this in deadly coronaviruses for man.
In Steven Soderbergh's Contagion (2011), a Chinese virus causes influenza with a 30% mortality. But a researcher finds the vaccine by injecting it herself and verifying that it is effective. The movie is pretty realistic in terms of social reactions, but science doesn't get vaccines like that. The question on everyone's lips now is: when? "A vaccine takes four months to develop, but its safety must first be evaluated so that it does not produce harmful side effects," replies Enjuanes. "As much as the controls are shortened, it will take six or maybe eight additional months to confirm it, a week or two is not enough." The version of the coronavirus reconstructed in his CNB laboratory carries the antigen that invokes immunity against the virus. But it must be evaluated first in laboratory animals, in this case humanized mice (with human genes).
This technology allowed the team of Enjuanes and Isabel Sola (also a virologist) to become the first in the world to create a synthetic version of a coronavirus. The mice in his lab are now protected against the two deadly coronaviruses, the one that caused SARS and MERS-CoV. "You have to have the potential to take it outside the mouse, in higher animals, like macaques," says Enjuanes. "But in Spain there are no laboratories with macaques. For that you have to collaborate with foreign teams ”. Isabel Sola, co-director of her laboratory, estimates that in the best case it would take between 12 and 18 months to have the vaccine ready.
The battle against the Wuhan virus can be won in a shorter time if we have antiviral treatments that slow the progression of the virus in the sick. And if there is hope now, we owe it exclusively to the anticipation of scientists. In the past they have opted to dedicate the scarce resources available to them and the best of their intelligence to fight against pathogens that nobody cared about, in the midst of political disinterest, regardless of color. Thanks to this far-sighted ant work, the Spanish arsenal has a front-line weapon: Aplidine, originally developed by PharmaMar for a type of leukemia. "We tested it in coronavirus cell cultures and saw that the reduction in virus replication was dramatic, even in very small doses," says Enjuanes.
Isabel Sola explains that the successfully neutralized coronavirus is not that of Wuhan that is now circulating on the street (it did not exist then), but a first cousin that infects humans. It uses the same protein (between 96% and 98% similar) that Wuhan virus needs to raise offspring within cells. Aplidine latches onto this protein like a stick that clogs the wheel of viral reproduction and derails it. "What we hope is that a similar effect will be seen with the new coronavirus, and that is what we want to verify," says Sola.
The current collaboration between working groups to obtain a vaccine is a good example to move forward efficiently "
Isabel Sola, at the CSIC headquarters of the Autonomous University of Madrid./ ALFREDO CÁLIZ
Aplidine is already a safe and approved drug. It can be manufactured in large quantities. If you neutralize the new coronavirus, patient clinical trials could be accelerated. It would not be unthinkable to have a therapy later this year, says this researcher.
The third way consists of the serums of people who have been cured. Many recovered patients had blood drawn, and the sera, although not abundant, contain antibodies that neutralize the virus in the infected. Enjuanes remembers the Ebola crisis, with the missionary doctor who was brought to Madrid and who died, and the contagion of the auxiliary Teresa Romero. “Teresa was evolving very badly. One night we thought he was going to die. Serum was administered from a nun who was helping the missionary father, and who had recovered after infection, along with an antiviral. And the next day Teresa began to survive. " Ebola is far more deadly than the new coronavirus.
The fourth way relies on genetic engineering to design monoclonal antibodies ... thanks to scientific instinct. Enjuanes and Sola have previously demonstrated the effectiveness of specific antibodies made by a Dutch laboratory that prevented the death of mice infected with a Wuhan-like coronavirus, even 24 hours after infection. The antibodies interfered with a part of the geography of the spicule that forms the crown of the virus, essential for it to enter and infect human cells, and which is common to that of the Wuhan virus. That has given rise to a European project where Spanish researchers hope to repeat the neutralizing success of infecting animals with the new CoV-2. "It's like immunotherapy," adds Sola. "The project includes the test in healthy people to verify the safety of these antibodies", easy to manufacture in large industrial fermentations.
But clinical research needs money and time. And although urgency now magically brings in funds that did not exist in the past, scientists need to produce enough animals first in sufficient numbers - something that could happen this summer - a couple more months for experiments and the involvement of pharmaceutical companies. to produce the antibody on a large scale. "It is a project designed for two years."
Mariano Esteban is a veteran virologist at the CNB who is very aware of the pandemics that have historically devastated humanity in his daily work. Not in vain does it belong to the WHO commission that meets every year to decide what will be done with the smallpox virus samples, confined in two high-security laboratories, in the United States and in Russia. Smallpox is the greatest killer of all. But two centuries ago a Spanish doctor, Xavier Balmis, launched a worldwide vaccination campaign for its eradication, using the fluid from the pustules on the hands of cowgirls who milked cows infected with the vaccine form of the disease.
We are in the final phase of vaccine production ”
The researcher Mariano Esteban, at the headquarters of the CSIC of the Autonomous of Madrid./ ALFREDO CÁLIZ
At the time it was unknown that the fluid actually contained the vaccinia virus, which conferred immunity to man, Vaccinia virus - a poxvirus. Esteban and his team have followed in Balmis's wake with their own technology and have used it as a powerful agent to vaccinate: they disguise it with the proteins of another very aggressive virus, cultivate the variants and select the one with the most power. In this way, they have made vaccines against agents as fearsome as Ebola, or viruses such as Zika or Chikungunya, without forgetting HIV. In many cases, this technique has successfully immunized laboratory animals with protection levels of up to 80% and 100%. When the coronavirus emerged in Wuhan and its genetic sequence was made public, Esteban's team already had the technology ready. They went to work to create the design of a hybrid between a highly attenuated variant of the Vaccinia virus and the coronavirus, robbing the latter of the spike that serves as a hook to enter human cells to infect them.
"We are always at the foot of the canyon to counteract any infectious process," recalls Esteban. "So when the sequence was published we went to the databases, looking for the most relevant virus protein that elicited an immune response. We contacted a German company that manufactured synthetic sequences and sent our insert vector with the coronavirus sequence design. We wanted to insert the coronavirus genes into our attenuated virus, and we finally received the sequence in three weeks. ” The design is now ready. Now the virus cultures remain and select the most promising variants, as a good farmer does. "We are in the final phase of vaccine production," says Esteban. Then it will have to be tested on animals and then on humans. It will be necessary to generate "several thousand vials to test healthy people and check that neutralizing antibodies are produced."
The second stage will extend the trial to a greater number of healthy people exposed to the virus, "especially health and family members of infected people", to demonstrate that it is safe, effective and that it produces immunity. The last phase, if the data is positive, is the most desired: manufacturing the vaccine in large quantities "to immunize thousands of people." But it will take quite a few months, says this veteran virologist.
Esteban has envisioned critical scenarios with smallpox in mind, but admits that the far less deadly new coronavirus has turned out to be ahead of science ever since it appeared. "It surprised us all." Remember the images of the Chinese manufacturing field hospitals in just two weeks. “They isolated a city of 11 million, it was somewhat shocking. Those containment measures were very strong back then for a small number of deaths and cases, but they anticipated it. ”
Esteban believed that at first the outbreak could be contained. There were the precedents of the SARS and MERS viruses, with much higher mortality rates. A situation in Spain like the one we are now experiencing was nothing short of unthinkable. “You could think of isolating groups or zones, as happened in the Canary Islands at the beginning, but not this. All virologists have surprised us and we have to learn more about the biology of the virus: how it multiplies, its mutation rate, how it interacts with our defenses and why it is so easily spread. ”
The virus has won this first round, but now comes the counterattack of international science. The race to get a vaccine has accelerated dramatically and behind a flow of hundreds of millions of dollars looming several candidates. Those in the front line are testing themselves to see if they are safe. CanSino Biologics and the Beijing Institute of Biotechnology test a prototype in 108 candidates based on a non-infectious viral vector, in a first phase to verify the safety of the vaccine. The University of Oxford tests another similar vaccine in 510 healthy people to verify safety and also efficacy, only that the non-infectious vector is derived from chimpanzees. Americans have begun clinical trials on 45 healthy volunteers with a vaccine that is based on the coronavirus RNA segments that code for the spicule that it uses when attaching to cells. There are other candidates that work well in laboratory animals. But most agree that it will take at least a year or more for the vaccine to reach humans.
However, the good news is already looming. The drug Remdesivir from the pharmaceutical company Gilead is showing effectiveness in the preliminary data of a study with more than 500 patients in China. And hydroxychloroquine is proving effective in some patients.
José Antonio López Guerrero (JAL for locals and strangers), virologist and director of the neurovirology laboratory at the Autonomous University of Madrid, has a small team, with far fewer resources than other large research centers. “I honestly did not think that what was happening in China could be transferred here. Not even with the first foci in Italy. Most virologists have been surprised at how quickly the virus has spread. I had been traveling asymptomatically long before. ”
Most virologists have been surprised at how quickly the virus has spread. I had been traveling asymptomatically long before "
The virologist José Antonio López, portrayed at his home during the quarantine./ ALFREDO CÁLIZ
JAL and his team have found that a very effective antiviral against the herpes virus dramatically inhibits a type of coronavirus alpha that causes a cold, and that it is very similar to the new coronavirus. "It has a similar lipid cover", explains this researcher, author of the book Virus, neither alive nor dead (Guadalmazán). The drug, characterized molecule by molecule, inhibits the replication of this virus in laboratory cell cultures, destabilizing the fat covering. The patent will be filed soon and the results will be published.
For years, investigations have been held back for lack of money, although JAL's group has received private funding, allowing it to survive. To develop a therapy against the Wuhan virus it is necessary to work in high security facilities for this type of microorganisms. But there is hardly any in Spain. International cooperation is needed. For small research teams, the first stumbling block is access to these highly secure laboratories.
Animal studies are the necessary pre-stage before conducting human clinical trials. But this case, a potential coronavirus therapy worth checking out, is now up in the air for lack of resources. "Small groups are like skinny dogs, everything turns to fleas," says JAL.
The origin of the virus remains to be determined. Bats have a coronavirus whose genetics are 96% similar to the new Wuhan virus and target the natural repertoire. But that 4% difference, in genetic terms, is an abyss. Humans and chimpanzees share 99% of the genetic sequence, but we are certainly not the same. And while it is known that China's wet markets sell bats in cages — Enjuanes knows these animal markets where there is a continuous exchange of feces and ensures that the smell is unbearable — something else was needed: an animal that functioned as a vector or bridge . But it was enough to jump the virus to a single person to start the chain of contagion.
It is vital to know from minute 1 of infection who has a very high viral load to separate these patients and treat them differently. "
The microbiologist Laura Lechuga./ ALFREDO CÁLIZ
And now, to win the war, you have to draw a geographical map of infections. The rule is: tests and more tests to see who is infected and who is not, even if they have not developed symptoms, and to establish the necessary quarantines and isolates. "A greater number of tests implies better and greater control, because all those who are infected could be identified (even on day 1 of infection) and isolated to avoid contagion. There are a large number of people who are carriers but are asymptomatic, and this is a big problem, ”says Professor Laura Lechuga, from the Catalan Institute of Nanoscience and Nanotechnology (ICN2) in Barcelona.
Lettuce, a microbiologist and researcher, coordinates the development of two types of biosensors within a European project, CONVAT, which can revolutionize tests in one year. The idea of a biosensor is similar to the meter that many diabetics use to find out the blood glucose level. Only in this case, what is analyzed is the fluid from the patient's mouth, nose and pharynx, since the virus is not in the blood, explains this researcher. The biosensor carries specific antibodies that detect if the patient is infected with the virus. It would take half an hour to answer your questions and you would not need specialized personnel to do the test. "It's like catching the virus," says this researcher. But to avoid a false positive or negative, a second test could be done, just as quickly: a biosensor that uses DNA probes that identify the genetic sequences of the virus and more quickly.
In rare cases, it has been seen that the virus can re-emerge in patients up to 14 days after testing negative, perhaps by taking refuge in tissues where it escapes test scrutiny, although controlled by defenses. But it is a mistake to talk about reinfection of already immunized patients, explains Luis Enjuanes. Precisely the new biosensors open a door to check the state of our defenses against the next waves of the new coronavirus. "My forecast, for quite a few weeks, was that this virus had possibly come to stay, and I still think that the same will happen with the flu, which is seasonal," says Enjuanes.
"We are going to end up beating him, I have no doubts," says Isabel Sola. “But winning the first round is not the same as winning the tenth. Containment measures will have their effect. With the summer, more light and higher temperatures will prevent it from transmitting so easily, and that will play in our favor. And if the virus emerges next winter, there will be people who have immunity. " In that assault we will have more weapons to win it.
The enemy is tiny and invisible. "The solution will be 100% scientific", concludes Mariano Esteban.