Suresh Dhaniyala, Hema Priyamvada Ravindran and Shantanu Sur - The Conversation
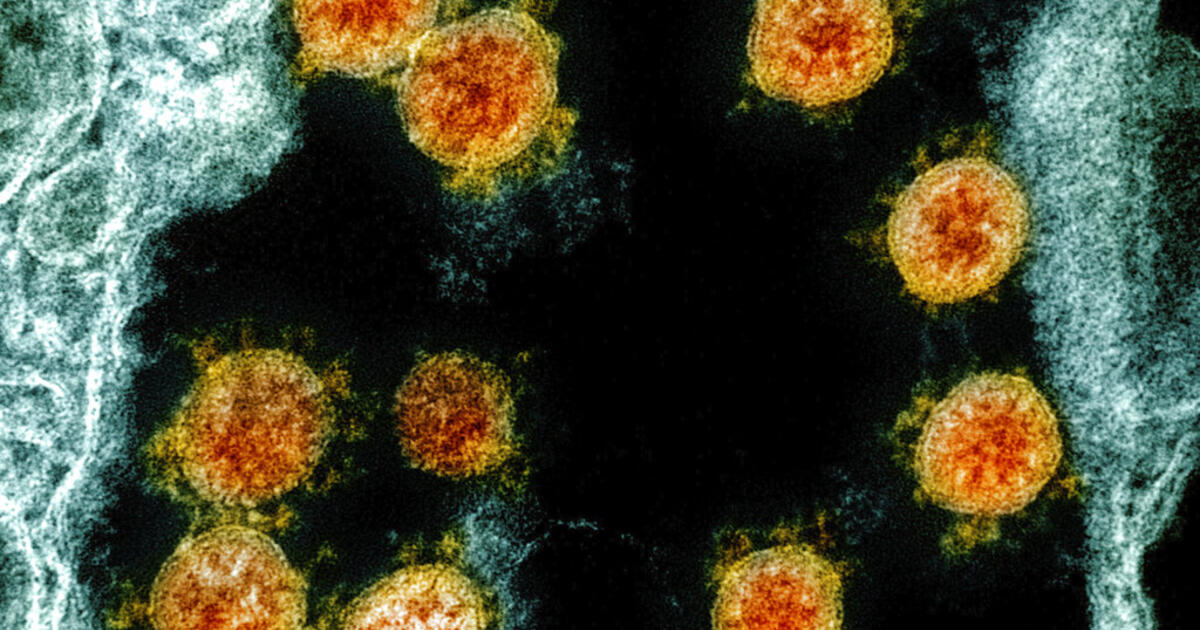
A growing body of research shows that SARS-CoV-2, the virus that causes COVID-19, can be transmitted from person to person through the air. Poorly ventilated indoor spaces in areas where the virus is prevalent are particularly dangerous.
In the fictional world of Star Trek , public health officials and first responders could instantly determine if a space had a dangerous concentration of airborne viruses and any other pathogens, simply by moving a tricorder .
That technology, imagined 60 years ago, is still firmly in the realm of fiction . However, several research labs are working on devices that can rapidly detect specific pathogens in the air, including SARS-CoV-2.
The air we breathe
Detecting the presence of virus particles in the air is complicated by the mixing of other particles in the air. The atmosphere includes a large number of floating particles, a significant fraction of which are biological. Normally, with each breath, you inhale about a thousand biological particles.
[Do you smoke? WHO links cigarette smoking to increased risk of complications from coronavirus]
These bioaerosols include living and dead organisms, including viruses, bacteria, fungi, pollen, and plant and animal waste. Viruses are the smallest of these particles. They range in size from 10 to 300 nanometers, or millionths of a millimeter. In contrast, red blood cells have an average diameter of 6 to 8 microns, or 6,000 to 8,000 nanometers. Bacteria range from 1 to 4 microns and fungi from 5 to 10 microns. Plant and animal debris are generally larger than 10 microns.
Most of these biological particles are not a health problem, because most are fragments of plants and animals, including humans. However, it only takes a small number of dangerous microbes to produce a pandemic.
Bad News Microbe Identification
To understand the potential threat of bioaerosols, it is important to identify the small fraction of pathogenic or troublesome microbes among all bioaerosols present. Bioaerosol identification begins with capturing biological particles from the air, typically collecting particles on a filter, in a liquid vial, or in hydrogels.
Often times, researchers transfer the collected bioaerosols to a culture medium designed to support the growth of microbes. The way the microbes respond to a specific culture medium (the size, shape, color, and growth rate of the microbe colony) can indicate the species of microbe.
[FDA authorizes emergency use of blood plasma against coronavirus]
This process can take several days or weeks and is often ineffective. It turns out that scientists can only identify about 1% of the microbes in the air with this approach.
Increasingly, scientists rely on gene-based analysis to map viruses and other microorganisms collected from air samples. A popular technique for gene-based analysis is the polymerase chain reaction (PCR), which uses an enzymatic reaction to make many copies of a specific gene or a portion of a gene so that the genetic sequence (DNA or RNA ) can be detected in a sample. A PCR test can be designed to detect specific gene sequences of a microorganism so that the detection of the sequence equals the identification of the microorganism.
This technique is currently the standard for detecting the presence of SARS-CoV-2 from nasal swab samples. PCR-based methods are very accurate in identifying pathogens.
Next-generation sequencing technology makes it possible to rapidly sequence entire genomes of organisms. Using these techniques, researchers now have the ability to understand the entire population of microorganisms, their diversity and abundance, in the air.
Fast detection
Despite these advances, much work remains to be done to instantly identify the presence of airborne pathogens. Current techniques for identifying microbes are expensive, require specialized equipment, and involve lengthy processing steps. They also cannot detect a species from small amounts of genetic material.
Recent advances, however, show promise for the development of sensors that can provide rapid information on bioaerosols.
One approach uses laser-induced fluorescence. In this technique, the particles are illuminated with light of a particular color or wavelength, and only the biological particles respond by fluorescence or emission of light. This technique can be used to identify and quantify the presence of biological particles in the air in real time, but it does not differentiate between a safe and a harmful microbe .
With laser-induced fluorescence, the particles are illuminated with light of a particular color or wavelength. Jan Pavelka / Wikimedia Commons, CC BY-SA
Another advance is the use of mass spectrometry for the detection of bioaerosols. In this technique, a single bioaerosol particle is separated with a laser and the molecular fragments are immediately analyzed to determine the molecular composition of the particles. The researchers are also using sensors based on Raman spectroscopy. Raman spectroscopy can identify molecular composition from light reflected off samples without destroying the samples.
Big challenge in a small package
These techniques are advancing in the instant detection and identification of bacteria and fungi in the air, but are less efficient in detecting viruses, including SARS-CoV-2. This is mainly because the viruses are very small, making them difficult to collect with air samplers and difficult to perform PCR analysis given the small amount of DNA / RNA.
[Coronavirus becomes the third leading cause of death in the United States]
Researchers are working to address the limitations of airborne virus detection. In our Clarkson University laboratory, we have developed an inexpensive bioaerosol sensor and collector for large-scale bioaerosol sampling. This battery-operated sampler uses a micro-sized high-voltage source to ionize viruses, bacteria, and fungi in the air and collect them on a surface. Ionization gives biological particles an electrical charge. Giving the collection surface the opposite charge causes the particles to adhere to the surface.
Samples from our collector can be analyzed with new portable DNA / RNA sequencers, allowing near real-time bioaerosol detection with low-cost portable equipment.
Where is my tricorder ?
These advances could soon make it possible to detect a known pathogen, such as SARS-CoV-2, with a wearable device. But they are still far from being a tricorder.
For one thing, they require relatively high levels of a pathogen for detection. Being able to identify a virus like SARS-CoV-2 at lower levels that are nonetheless sufficient for disease transmission will require the development of sensors with lower detection limits. Additionally, these sensors can only be customized to detect specific pathogens, not to search for all possible pathogens.
Although the equivalent of the tricorder in Star Trek is not around the corner, the need for such a device has never been greater . Now is an opportune time for the emergence of new detection techniques that take advantage of the spectacular advances that are being made in the fields of electronics, informatics and bioinformatics. When the next new pathogen emerges, it would be nice to have a 'tricorder' on hand.
This article was translated by El Financiero.