By Liz Szabo—
NBC News
After decades of good news in the fight against cervical cancer and a steady decline in cases and deaths, a new report suggests that some women are not part of this trend.
Thanks to early detection and treatment, cervical cancer rates have been reduced by more than half in the last 50 years.
Rates are falling most rapidly among women in their early 20s, the first generation to benefit from the Human Papillomavirus (HPV) vaccines, approved in 2006.
HPV causes six types of cancer, including cervical cancer.
Among women ages 20 to 24, the incidence of cervical cancer fell 65% between 2012 and 2019, according to a report published last Wednesday by the American Cancer Society.
“Cervical cancer is one we know the most about,” explained Dr. Nicolas Wentzensen, a senior investigator in the clinical genetics branch of the National Cancer Institute, who was not involved in the new report.
“We have made amazing progress and continue to see a success story.”
However, not all women are benefiting from that progress.
The overall rate of cervical cancer among women of all ages has stopped declining.
A generation that is not benefiting from vaccines
Among women between 30 and 40 years old, the incidence has been increasing.
The diagnosis of cervical cancer among those aged 30 to 44 years increased almost 2% per year between 2012 and 2019.
“We have to make sure we don't forget about that generation that was too old for HPV vaccination,” urged Jennifer Spencer, an associate professor at the University of Texas-Austin Dell Medical School.
Fortunately, the cancers detected in women between 30 and 40 years old were mostly early, curable tumors, said Ahmedin Jemal, lead author of the new report and senior vice president of surveillance and health equity science at the Cancer Society.
About 13,800 women in the United States are diagnosed with cervical cancer each year.
About 4,360 die from this disease.
Many women are not screened
The researchers did not delve into the reasons why cervical cancer is becoming more common in some women, Jemal said.
But medical testing rates may play an important role, said Spencer, who was not involved in the study.
These allow doctors to detect and remove precancerous lesions before they become cancerous.
According to the Centers for Disease Control and Prevention (CDC), more than half of women diagnosed with cervical cancer have never been screened or have not been screened in the past five years.
Studies show that fewer women are receiving routine cervical cancer screening.
According to the National Cancer Institute, the number of women ages 21 to 65 who have been tested according to the latest guidelines has fallen from 87% in 2000 to 72%.
Other research has revealed that women aged 21 to 29 were the least likely to be up to date on their check-ups, with 29% behind.
Women who are non-white, uninsured, living in rural areas, and those who identify as gay, lesbian, or bisexual were also more likely to be behind on their exams, according to the study.
The importance of the Pap test
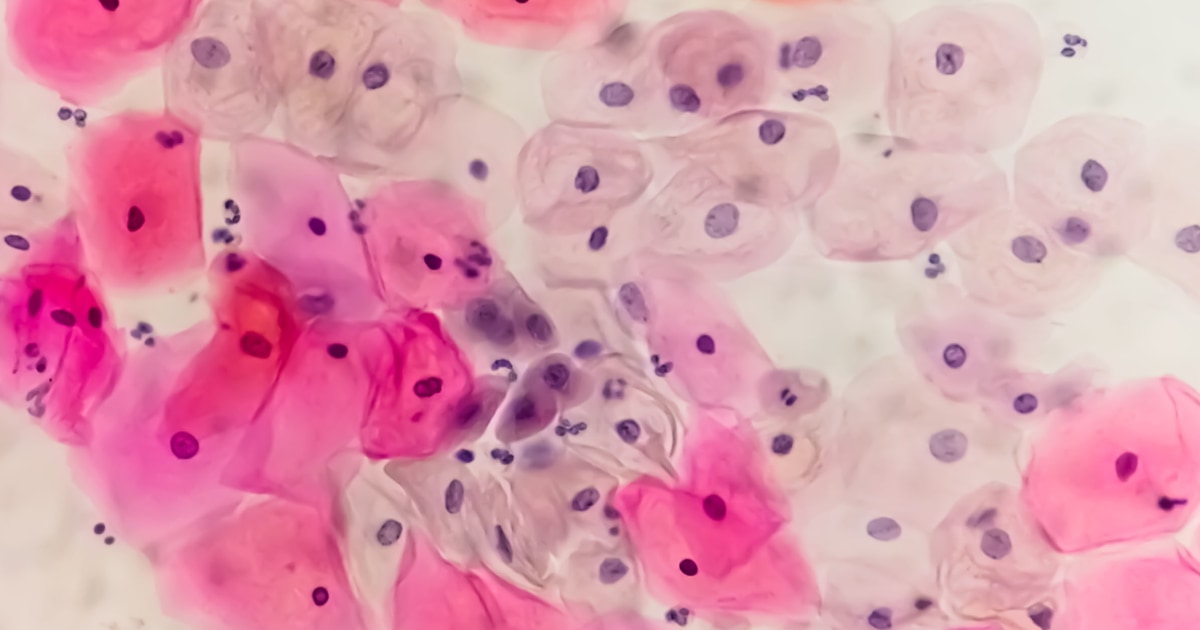
The U.S. Preventive Services Task Force recommends that women ages 21 to 29 have a Pap test — which examines cells under a microscope — every three years.
Those between 30 and 65 years old can get tested every three years, an HPV test every five years, or a combination of the two.
The latter can detect genetic material from the Human Papillomavirus.
Spencer said it's possible that low testing rates among women in their 20s help explain the slightly higher rates of cervical cancer among women in their early 30s.
When women in one of Spencer's studies were asked why they had not been screened recently, they generally responded that they did not know they should or that no doctor had recommended it.
Only 1% of women ages 21 to 29 indicated they had skipped screening because they had received the HPV vaccine.
“It's clear that more patient education is needed,” said Dr. Betty Suh-Burgmann, chair of gynecologic oncology at the Kaiser Permanente Northern California clinic.
Her health system reminds women about their checkups through postcards, letters and phone calls.
This year, Kaiser Permanente will also begin texting patients.
The changing guidelines on cervical cancer screening may also have confused women and health care professionals, according to Spencer.
Until the early 2000s, most doctors gave women annual checkups.
The task force has updated its guidelines three times in the past two decades and is revising them again.
Others say the rise in cervical cancer rates among women in their 30s and 40s has no easy explanation.
According to Wentzensen, cervical tumors tend to grow slowly and often take a decade or more to progress from pre-cancer to cancer.
According to him, there may be other factors at play.
For example, the doctor wonders whether the number of women moving to the United States have not been screened, putting them at greater risk.
For his part, Spencer noted that
screening tests are only the first step in saving lives
.
Women with altered results should undergo additional testing and, if necessary, treatment.
In a study published last year in the American Journal of Preventive Medicine, Spencer and her colleagues found that only 73% of women with impaired screening results received follow-up care.
“The health system has a responsibility to think about who is falling through the gaps,” Spencer said.