They tear up at the sight of patients who die without their relatives, hurt the shielding force, and the anxious to bring the virus home • The Corona crisis has put doctors and nurses on a new front, demanding great mental and physical cost • Nurse: "Don't know what is going on every day, I'm stressed out the time"
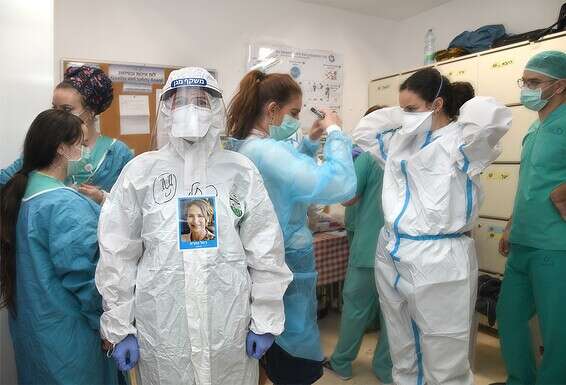
Post-Trauma Medical Staff // Photo: GettyImages
On March 21, Saturday, a week after Israel entered the Corona Restrictions, Rachel Gemara, an experienced nurse, worked on an evening shift at Crown A ward at Shaare Zedek Hospital in Jerusalem.
She sat in the army, looking through the screens at her patients eating dinner, and suddenly noticed something was happening to one of the patients, who had arrived in a serious condition a week before.
"It was 88-year-old Aryeh Even. His monitor suddenly started to twitter. I couldn't get in right away because I have to wear the protective suits first, which is a long time. His family was not allowed to stay by his side because of the virus, and he was all alone.
"In a few seconds the other patients left their dinner and went to hold him by the hand. They said 'Shema Israel', they didn't let him die alone. I see all this on screen while I dress - and cry. It was very hard for me not to be there , Next to it. " Ibn was the first Corona patient to die in Israel.
Rachel (33) has been working in the oncology department of the hospital for ten years. When they asked for volunteers for the new Corona Department, she immediately showed up. "I saw this as something important, a national mission, to give myself. We didn't know why we were coming in. Even now I'm proud of what I do, but seeing passing through the camera is a very difficult experience."
She is single, living alone in Jerusalem. The harsh pictures accompany her even when she returns home. "There were days I couldn't fall asleep. The things you experience in the department affect you mentally and mentally. We work 12-hour shifts, so my life is work, there's nothing beyond that. There are a lot of patients, and we have a lot of responsibility, because supervision is done remotely and needs to be put Heart for every detail. Don't know what is going on every day. Don't know how long it will last. I'm stressed and tense all the time.
"It's hard to see adults alone, without their families. We became like family to them. Beyond that, the protective suits make it very difficult to breathe and move. Every action takes a lot of time, and sometimes we race against time. The patients see only our eyes, not another part.
"With the adults the communication is difficult. They find it difficult to understand what I am saying and they cannot always identify me, which scares them."
The late Aryeh Ibn was a Holocaust survivor, and his separation reminded Rachel of the separation from her grandparents and private grandmothers, also Holocaust survivors of his age, whom she had not seen for many weeks. "I miss them, I think a lot about them. When I take care of older people, I think my grandparents could have been in that situation too. It connects me to them, and I call them more. To my grandmother the corona is flooding memories of the Holocaust camps. She tells me about them on the phone. "
A week later, she experienced an event she will never forget, this time with a happy ending." One night, a 51-year-old man with no background illness arrived, whose breathing was problematic. I was alone in the ward, armored. The rest of the crew was outside, in the army.
"The man asked me for help, and then, all at once, he collapsed with my hands. I immediately put him on a chair and saw that he was losing consciousness. It was the most stressful moment of my life. He stopped breathing in front of my eyes. And I'm there alone, his life depends on me.
"I had to leave him for a few seconds and run to get a high-concentration oxygen mask. I wanted to get the mask and put it in immediately. After 20 seconds, he regained consciousness. He opened his eyes and went back to breathing himself. I kept thinking what would have happened if I hadn't been there at that moment.
" This patients can deteriorate in front of your eyes without warning. It is stressful. We have to be careful and pay attention to everything.
"The next two days, that person could barely get out of bed. It was really hard for me to see him like that. Later we moved him to the intensive care unit. After I said goodbye, I stood in the corridor and cried. I was afraid he wouldn't come out of it, I saw what the disease was doing to people. So basic we were excluded from people, even young people.
”In the end, he recovered, miraculously. When he was released from the hospital, he came to thank me. He stood outside the glass door and said, "You saved my life." I replied that I was so happy to see him like that, to know that he was recovering. Seeing someone who was in a difficult situation and recovering is an amazing feeling.
"Also to see how the ill patients help the hardest warms my heart and gives a lot of light. To see a doctor who comes in in the middle of the night to become a patient in his bed. See how the auxiliary forces hold the patient's hand and sing to them. We make every effort to feel that they are not alone. The hospital management supports us and strengthens us. "
"I have a sense of deja vu," says Gali Weiss, 55, the hospital's vice president responsible for 1,700 nursing staff, "I served permanently in the medical corps. 15 years ago, when I served as head of emergency preparedness hospitals in the Home Front Command, I participated in writing a hospital preparedness plan for a biological attack on Israel. We then talked about SARS, Avian Influenza, Anthrax. No one dreamed of Corona.
"This crisis allowed us to check the reality we wrote in reality. From the beginning of March, when we set up the department, I got up every day at five in the morning and returned home at ten in the evening. On the way to the hospital and back, I kept thinking about how to improve. I went over the exercises that we did in the army, Repeat.
"There was a real difficulty in adjusting the reality to the exercises, because this virus is something new. With the few hours of sleep I had every night, I didn't sleep well, I dreamed we weren't working the best. I had nightmares. "
According to Weiss, more than 20 brothers and sisters in the gates of justice fell in Corona, all of whom became infected in the community - that is, not as a result of their work at the hospital." I felt the need to call everyone and ask how they were doing. There is one brother who is unclear how he contracted. Unlike the others, the possibility of being infected in the hospital cannot be ruled out. He was in serious condition.
"I talked to him every day on the phone, but one day I decided to defend myself and go into the department to get him a gift from the team. After ten minutes, I felt like I was no longer able to. I sweat and see nothing through the glasses. I asked the nurses, 'How do you work like that?' "It was hard for me to see him in this situation. I constantly worry about my teams."
As the load and pressure increased, Weiss convened the nurses to meet with a psychologist. "We wanted to give them tools to deal with the situation, to talk about their feelings. When it was my turn to talk, I broke down. I have a mother who is dealing with a serious illness. She is at home in Tel Aviv, nursing, with a close but clear nurse. Every Friday I take her in the chair Wheels for a coffee shop For the past two months I have come to meet her outside the door, we celebrated her 80th birthday in the distance.
"I'm assuming I'm a carrier of the disease, because of the constant exposure to the hospital. If I approach her and catch her, it will sit on my conscience. This was the first time I cried, after not hugging my mother for seven weeks."
Do you feel the team is under increasing mental pressure?
"There were a limited number of excellent nurses in the Crown who were not under pressure, although some came from intensive care units. The pressure in this department is different. Out of concern for our health, we have returned them to their parent wards. In recent days, as we re-evaluate following the improvement, we asked who would like to continue In the department. Everyone wanted to, and it warmed the heart. "
What is the difference between the Corona and other difficult events you have faced in the past?
"We are studying multi-casual events. The most difficult event also begins and ends, followed by a return to routine. The Corona, on the other hand, is a rolling event. Don't know when it will end and how it will develop."
Even on routine days, medical teams deal with difficult mental states. The Corona puts them on a new and especially stressful front: high-intensity work with little-known virus, necessitating a professional response to dynamic situations involving rapid deterioration of patients, lack of protective equipment, and especially around-the-clock work in long, demanding shifts.
In letters sent by doctors' committees to the management of the HMOs in Israel at the beginning of the crisis, it was first written that doctors report mental distress. A preliminary study by the School of Behavioral Sciences at Tel Aviv Academic College and Ichilov Hospital in late March found that 18 percent of public hospital doctors reported anxiety during this period, 30 percent reported burnout, and 10 percent reported depressive symptoms.
"The study is the initiative of Dr. Eden Schusterman, my intern," says Prof. Jacob Ablin, Director of the H-Internal Department in Ichilov. "By March, the tsunami was known to arrive. It was a very stressful time, and we wanted to test the doctors' feelings in real time, to see if it was possible to predict who would be depressed, and if things could be prepared in advance.
"The most interesting finding we came up with is that as you enter the fray with high levels of burnout, it increases your sense of depression. Coping with burnout by a physician and medical staff not only increases quality of life, but also improves coping with emergencies. Burnout and depression can impair ability Of the physician to provide optimal care.
”Another interesting finding in the study comes from a comparison of doctors in different departments. In the inner wards, who had to stand in the front line of the epidemic, there were more doctors who reported anxiety than in the intensive care units, where they were more accustomed to such situations. Incidentally, the major cause of anxiety in most participants was the concern for their parents, not their children or themselves. It's an exciting find.
"We looked at what could reduce anxiety levels, and things like trainings on respirators (less internal doctors regularly use respirators, whatever new ones have been used to use; the E) and reducing bureaucracy. Knowledge reduces anxiety.
"I was under pressure too. The solution was to talk about it. To be with them. To talk. Just to be together as much as possible. Some of the time we were isolated from each other, so we talked on the phone. There were many one-on-one conversations, giving legitimacy to feelings and concerns."
Doctors do not like to talk about mental distress caused by their work. But the realization that the distress exists, and even intensified during the Corona, spurred hospitals and the Ministry of Health to open "hotlines" to doctors, with complete anonymity. The Eran Foundation (Mental Health Assistance) also opened two hotlines, which operate 24 hours a day - one with the Medical Association, and the other with a general health fund. At the same time, an online service runs inquiries.
"Doctors have double distress," explains Dr. Shiri Daniels (49), a national professional director of ERN and a member of the Health Ministry's Suicide Prevention Council, "They experience difficulties because of the nature of work, and difficulties because they are people with their own regular problems. The distress is even threefold, because doctors also have a built-in difficulty to talk about their feelings and to seek help. So we thought of a dedicated line that would allow doctors to evacuate without revealing their identity. We assumed that medical professionals would prefer to expose their feelings outside the health care system.
"When a person feels listened to, he no longer has to be the hero doctor, the Superman, and that also increases the willingness of others to evacuate. They know that everything is confidential.
" The medical teams work under difficult conditions. They constantly support others, and finally find themselves powerless and exhausted. They are worn because of the harsh conditions, and do not always feel that the system backs them up. This is a population that rarely turns to help. They also don't have when, they often work 26 hours in a row. Even if a doctor feels distressed, who will he refer to and when? Within the system it can be perceived as weakness and cause them harm.
"Previous research, following the SARS epidemic in 2002, has shown that medical teams have experienced an increase in symptoms of anxiety, depression and irritability. In the current crisis, we realized that we had to open a dedicated line of doctors in real time."
Eran's Corona Lines for Doctors opened in early March. The number of referrals increased on average from four a week to 15, and Dr. Daniels said there was an increase in referrals as well. "The Corona has intensified the clutter and erosion, and also the catch between work and family, because of the fear of catching up with the household members."
Dr. Zvi Fishel (58), chairman of the Israel Psychiatric Association and who established the Eran line for medical federation doctors, says that "physicians generally refrain from receiving physical medical treatment. If a doctor feels unwell, he meets a colleague in the hallway and consults him along the way. This is also the case with mental matters. The feeling is 'I'll get along and know how to cope'.
"Our concern is that when the doctor gets to a situation where he can no longer cope, it will be too late. The suicide cases at Soroka Hospital in the past year have sharpened our problem and the need to provide mental help.
"During the Corona, everything is reduced. Also the burden, the coping with the difficult cases. Some of the doctors are new, and the danger to your life and your family life is a new feeling. Another difficulty lies in the ethical dilemmas that can arise if we lose control of the health system - for example, the difficult question Doctors want to know that there is a proper protocol for ethical decision-making and that the system will back them up at the end of the process.
"We are working to make the line accessible to every physician. We sent everyone a personalized SMS, and at the same time, we asked department managers to encourage physicians to seek help. "
Dorit Muscho Ben Simon, director of the employee experience department at General Health Fund, is the one responsible for opening ERAN's line to the HMO's medical staff. "Doctors tend not to seek help. In the professional language, we call it 'compassion exhaustion' - therapists who are exposed to human suffering, sickness, loss and trauma, dealing with a variety of stressors, whose accumulation can lead to exhaustion and negative consequences for the quality of care and the welfare of the therapist."
According to Dr. Daniels, 39 percent of the Eran lines were complaining about load, voltage and erosion. 33 percent cited anxiety from the virus, fear of infection, encounter with dreadful sightings of respiratory or deceased patients, pain and loneliness. 18 percent speak of pain and distress on a personal basis, and 10 percent cite other factors.
"There are doctors who come home and sleep in isolation, so as not to jeopardize their family, and that adds another difficulty, of distance from the woman and the children. We also received a call from a doctor's daughter, who is worried about her father, because he is an adult and is at risk.
"Remember that doctors do not get exempted from spousal and other problems we all have. The combination of sleep deprivation and lack of family support factors only exacerbates their distress. Regardless of Corona, suicide rates are higher for physicians than for the general population. ”
What training did ERN volunteers receive to address physician inquiries?
"We did a dedicated seminar for them, where there were meetings with doctors and conversations with department managers about doctors 'exhaustion and barriers in seeking help. We gave them a skill in identifying signs that needed mental help from doctors, because a doctor wouldn't call and say' I'm worn 'or' I have Nightmares, but will talk about the shortage of personnel or the lack of protective measures. When a doctor turns up, the volunteer has to locate the problem himself. We have prepared training kits for them, and we also give them feedback on every call.
"Some volunteers initially feared what doctors could offer, because The stereotype of an 'all-in-one doctor'. But when you realize it's a human being like everyone else - everything changes. Some of the applicants told them, "You don't know how much we are missing." Among the volunteers who handle medical staff inquiries are also doctors and nurses in retirement. "
Eti Shor (66), who was a primary nurse at Shaare Zedek and supervised by the nursing management of the hospital, is one of the volunteers on the ERN line for medical workers.
"I worked in the SARS and Avian Influenza and I know the distress, know what it is. At the time, when we were inside the patients' complexes, we would take turns every two hours. The work was in very warm protective clothing, and the most difficult is that it is very difficult to communicate with the patients. it is frustrating.
"When I receive calls from health workers, I can express empathy. As a nurse, I understand what they are talking about. I can also give professional tips and refer to relevant help centers."
What stories do you hear in conversations?
"A nurse says she comes in to take care of Corona patient, and he can't see her through the mask and shield. Tells me, 'He doesn't see me smiling, and I can't communicate with him, soothe him.' It puts her in mental distress.
" You died alone, without the family around him, and it flooded her with emotions. Another sister told how she was accompanied by an elderly woman from a remote room. I can really imagine the situation, "she gasps in tears." When the patient needs the nurse and she can't touch it, her compassion button works without her being able to do anything. It breaks. And on top of all that, of course there is the fear of bringing the virus home with you. "Is
there a difference between a regular call coming to Aran and a call coming from a doctor or nurse?
"Doctors and nurses who call not only talk about work, but also the depression of ordinary people. Doctors and nurses are also human beings, and each has their own distress. Everyone faces something in life."
Prof. Ehud Zamora (75) is one of the Corona's hotline volunteers. In the past, he managed the premature neonatal and intensive care unit at Soroka Hospital, and for 14 years he has been volunteering at Eran. During his Corona days he does this at least once a week. Some of the calls he receives come from the dedicated line of medical teams.
"One of the skills I acquired in my 40 years as a physician is communicating with people under pressure," he says. "The weight of work responsibilities is one of the major causes of stress for physicians, and this tension also takes home. Often, the physician's family goes down to second place in employment and attention. "I knew it about my meat."
How does the doctors hotline work?
"They have a special phone number, and when I get a call, I know it comes from the doctors line. In that situation, I can adjust the call to the doctor's special world. After all, I know the burnout, the pressures, the impact on the doctor and his family. The tension helps me manage the conversation. "
Is there a uniqueness to the problems that arise during this period?
"Mostly the fear of being infected, the fear of infecting the family, and the fear that they will be forced to stay in quarantine at home and not be able to help their friends. The other pressures are a little overdue. Doctors from the hot units say they are training because there is no break during a 12-hour shift.
" On the one hand, banging their heads is a risk group, and on the other, it does not release them from work. They must go. An experienced, experienced physician knows exactly what is going on in the disease like the corona, which adds to his stress.
"On the other hand, the shortage of manpower increases the commitment. So they have to put aside the concern and go to work, with all the tension."
On a routine day do doctors turn to mental help?
"Less than the entire population. Doctors feel vaccinated. The public gives them the feeling that they are 'superior' to life-related issues. It's an aura that accompanies them at work, and even when they leave it. It also adds a lot of stress. If I'm so appreciated as a doctor, I have to keep going And not to admit that I need help.
”When a doctor turns, he tries to have someone across the line understand his media. On the one hand, it is a matter of professional pride, and on the other, the need for someone to experience what they experience. When I face the turnaround, I bring with me all the dilemmas I have been through myself, and share it with him, who will feel he is not alone. "
Another psychological service is offered to doctors for free by the "For Tomorrow" association, which specializes in treating traumatized fighters on the battlefield. The association sees the Corona crisis as a battlefield, which can cause post-traumatic events in the warriors - in this case, the doctors and nurses.
And there are also private volunteer ventures, set up by doctors for doctors. "The quiet of Friday afternoon breaks the phone's warning beep," Dr. Reut Shoham, 45, wrote on her Facebook page, "Another doctor and another doctor want to talk. Ask for a link to the next group of zoom doctors. Want a moment for themselves. ”
Reut, Dr. of Organizational Psychology, accompanies medical teams at the health centers. "Taking care of caregivers," by definition, "because the system is very good at tasks, and less on people. They don't give them enough room."
When the epidemic broke out, and the hospitals went into emergency mode, Reut's work was halted. Dr. Shi Krontl (49), a family physician, suggested a group called "talking therapists" - an independent voluntary initiative, came to meet the online physicians who want to talk. They put together a team that includes four doctors and four psychologists, Zoom conversations between doctors.
" The degree of responsiveness of the doctors amazed me, "says Reut." We have several groups, each of ten doctors, who meet once a week for an hour. Every day a different group. At the beginning of the meeting everyone is anxious, embarrassed, and very quickly it becomes an island of security, a place to vent difficulties. When we identified a doctor with greater difficulty, we referred him to a professional. "
Krontel:" It's not mental health, but a safe space that allows medical teams to talk about what's really going on. Tell about the experience, say it out loud. The doctor's profession exposes us to other people's problems, and it's hard to do something that's not for the patient but for yourself. There is a fear what the colleagues will think of you. A desire to keep Pason, who would not be perceived as a coward.
"But such a group has power. Suddenly doctors share a wide range of emotions, which have arisen in different situations of the crisis. Sometimes they gasp in unexpected tears. Sometimes they say, 'I didn't even know that was what I was feeling.' Who dared to say things that were uncomfortable to say to anyone, not even to themselves. Mostly, they were glad to see that there were other doctors who felt like them. When we identified a doctor with great distress, we referred him to professional help.
"My concern is from the day after Corona. The Hi will end, the media buzz around the "Warriors on the first line" will fade, the adrenaline will go down, and the soldiers will be left with war or traumatic memories. During the war, mental defenses are mobilized to deal with the crisis, and functioning is maintained. When the crisis ends, a fall comes.
"The doctors, who were superheroes, would return to the grinding, gray routine, without the admiration and without the applause from the balconies and salutes. There will be a very big morale crisis."
Krontel says that this period also affected him personally. "I found myself short in my reactions, responding to patients with lacunae, and sometimes impatient, less able to contain. I'm afraid of this disease. It's not a paralyzing fear, but it does exist. In a banal throat test I did for the patient, I suddenly suspected she had a corona. Am I endangering myself? My family? '
"When I come home, I can't hug my kids before I change clothes and take a good shower. Although I am not depressed, the distress is there all the time.
"" The Corona is sowing considerable fear, "says Prof. Hezi Levy, director of Barzilai Hospital in Ashkelon." During the bombardment from Gaza, we knew how to turn from a normal hospital to a hospital under fire. We knew who the enemy was. Now it's an enemy you don't know or see. You are losing isolation staff - we have already lost 110 people who had to go into isolation in one day. You don't know who will infect you.
"I know it sounds weird, like we miss fights from Gaza, but the enemy here may be the person sitting in front of you, and you don't know it. You make decisions through screens."
Prof. Levy runs around the hospital and solves problems that arise before returning to the departments. "I gather all the knowledge I have to give solutions. Protect the staff and the patients, make decisions at a crazy pace every minute. Everyone looks at you, you have to be the responsible adult. It creates a lot of fatigue, stress, anger, a lot of things."
One of the brave decisions Levy made five weeks ago was to open a clinic for complementary therapies for staff. Because not only did the corona come from China, a good deal of complementary medicine, like acupuncture.
"I was exposed to Chinese medicine when I was chief medical officer 15 years ago," he says. "Recently, I was in China on a health ministry mission and learned how complementary medicine can be added to conventional care. "Diseases are one that incorporates different perceptions and touches on different aspects of the disease, including emotional ones. Such patients heal faster."
Prof. Levy recruited Dr. Gali Stupman (52), a pediatrician and Chinese medicine specialist, and after sending her to China, they opened a supplemental treatment center in the hospital last September - the second of its kind in Israel (another center operates at Bnei Zion Hospital in Haifa) "The center was offering Chinese acupuncture (which Stuffman does) and reflexology, which are included in the hospital and are free in the patient bed.
" The Corona stopped everything. On the other hand, as soon as occupancy in the wards went down, I initiated the opening of a supplementary clinic for the hospital staff, in support of this difficult and tense period.
"Complementary medicine tools can increase staff resilience and treat stress and anxiety, both emotional and physical manifestations. From the moment I received the hospital manager's approval to open the clinic to staff, I compiled a document with healthy lifestyle recommendations, nutrition , Supplements, etc., and we distributed it to all staff, along with an invitation to come and get treatment. "
Was there responsiveness?
"A few hours after we distributed the order, the secretariat at the call center informed me that the phone did not stop ringing. The journals were filled immediately.
" To date, we have handled more than 50 staff members each week. Now that the clinics are back with regular patients, I have found an alternative place to treat the staff, for at least the next month. "
What are the reports of staff members coming for treatment?
" Back pain, headaches, difficulty sleeping, irritability, tight shoulders and aggravation of chronic conditions. After treatment, they report very great relief. In the aggregate, after three treatments, there was a great improvement for them. "
Prof. Levy reveals that he himself went to receive treatment at the center." I had severe wrist pain. At the hospital, I was given two injections, but the pain didn't go away. Glee offered me an acupuncture.
"I showed up at the clinic, and she did the acupuncture with all the hygiene rules. I spent half an hour with the pins in my hand, and with the other hand I continued to work. The treatment helped me, the pain was gone."
The rumor of the successful center has also made its way into other hospitals in the country. In the past week, similar treatments have begun to be given to medical staff in several hospitals, in a limited format. The UK is about to launch a similar service inspired by the Israeli model, nationwide. Dr. Stupman says she received a call from the British Ministry of Health to advise the committee set up to do so.
"I advise them on how to build the system from a safety aspect. The medical staff is a risk group, they are more vulnerable than others to the dangers of the corona, so they must work optimally and adapt it to UK conditions. "
Timorhila@gmail.com