Safety or efficacy?
The vaccine dilemma 1:43
(CNN) -
With conversations heating up about the possible availability of a vaccine candidate, you may have heard the term "emergency use authorization," or USA, in the news lately.
But what exactly is it and how is it applied to vaccines?
Emergency Use Authorization is what the name suggests: a medical product that gets special clearance from the US Food and Drug Administration (FDA) for use during an emergency.
Sometimes it is a product that the FDA has already approved for another condition, and sometimes it is a new product that has not yet received the green light from the agency.
There is great concern and ongoing debate about whether any candidate vaccine should be granted an EUA, or full approval, without first completing phase 3 clinical trials of the vaccines.
Good news in the fight against coronavirus: possible treatments, vaccines and findings
Covid-19: Fauci sees risks of premature vaccine permission 1:09
911 emergency use authorizations
According to the FDA website, during public health emergencies, the agency may use emergency use authorizations “to help make medical products available as quickly as possible by allowing unapproved medical products to reach patients in need. when there are no suitable alternatives, approved by the FDA and available ”.
But that's only if "the known and potential benefits of the product, when used to diagnose, prevent, or treat the identified disease or condition, outweigh the known and potential risks of the product."
So, in essence, what an EUA does is accelerate the process of obtaining potentially useful medical products authorized for a specific use by the public during a health emergency.
This without the rigorous testing and subsequent scrutiny that is generally required to gain FDA approval, something that traditionally takes years.
When the health emergency is over, "then any US issued based on that statement will cease to be in effect," according to the FDA.
But the manufacturer can still submit documentation to the agency for regular approval.
US authorizes use of rapid test to detect coronavirus 1:21
The USA hasn't been around that long.
The process was embedded within the Project Bioshield Act, passed by Congress in 2004, which allowed the federal government to prepare and store new "medical countermeasures" during a declared public health emergency.
And despite having issued many USEs over the years, only one vaccine has received one, but it was in an unusual and controversial circumstance.
In 1997, the Department of Defense began a mandatory anthrax vaccination program.
Soon after, the soldiers claimed that the vaccine made them sick, for which they sued and a judge suspended the program, in 2003. The Department of Defense requested an EUA that later annulled the judicial sentence, in 2005, so that it could continue vaccinating personnel military, this time on a voluntary basis.
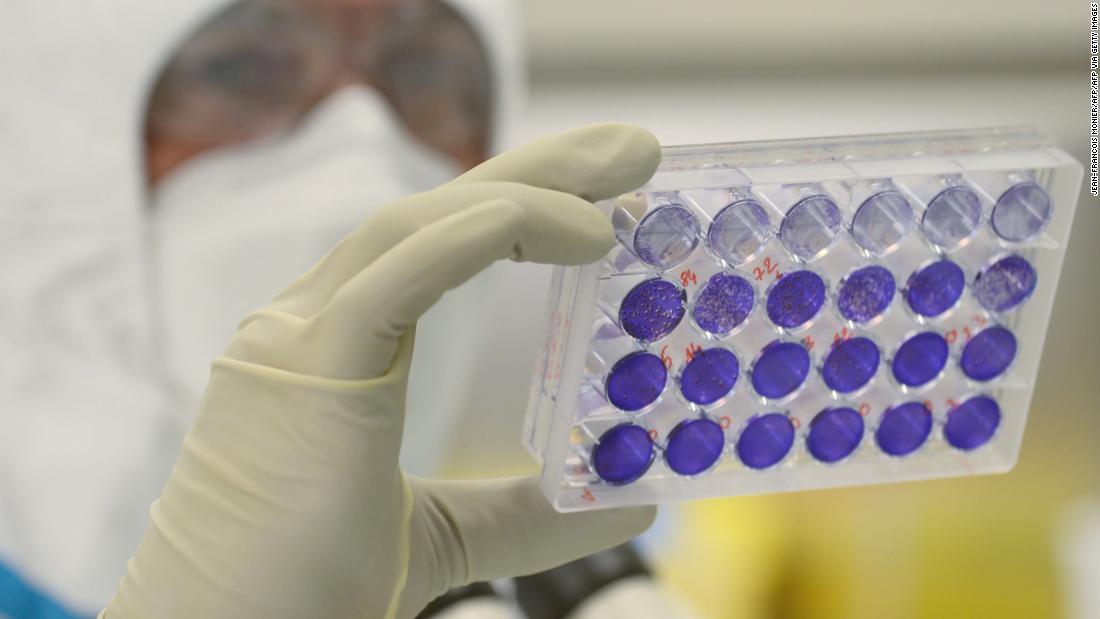
Emergency use approvals during the covid-19 pandemic
During the covid-19 pandemic, the FDA has awarded USUs many times to a wide range of medical products, such as respirators, personal protective equipment, including masks;
molecular and antigen tests to diagnose covid-19 and serological tests to look for antibodies;
and even treatments, such as remdesivir and convalescent plasma.
A USU can be revoked, as in the case of hydroxychloroquine and chloroquine.
These drugs had already been approved to treat and prevent malaria and showed promise against the new coronavirus in laboratory studies.
Initial small trials in COVID-19 patients added to the optimism, and President Trump touted the drug.
But larger studies found that the drugs are not effective in treating COVID-19 patients.
Additionally, one of the side effects could also be potentially dangerous in people who had pre-existing heart conditions.
After approximately two and a half months with the US, the emergency authorization was revoked.
The uncertain whereabouts of hydroxychloroquine in Brazil 2:35
Many experts find it problematic to grant an emergency use approval to a COVID-19 vaccine.
For one thing, vaccines are given to healthy people by choice, as opposed to drugs given to seriously ill patients who could die without them.
So drug makers have a higher bar, so to speak, to make sure there are no unexpected side effects that make healthy people sick, and the only way to find out is through large-scale trials, like the ones currently underway. taking place at the moment.
The FDA has said it would maintain a vaccine with a higher standard.
Dr. Peter Marks, who heads the FDA's Center for Biologics Research and Evaluation, said Thursday that the requirements will be more stringent than those for an emergency use authorization for an experimental drug.
"For us, for a vaccine for which there is adequate manufacturing information, if we are going to do an emergency use authorization, it will really be like one more emergency use authorization," Marks said at a seminar organized by the Margolis Center, from Duke University on health policy.
On Friday, Marks and FDA Commissioner Dr. Stephen Hahn said, in a joint blog post, that they would issue more guidance "shortly" on how much higher that bar could be.
They noted that it is the manufacturer's responsibility to apply to the FDA for an emergency use authorization or full approval, known as a Biologics License Application.
"With so much at stake, we understand the importance of being as transparent as possible about the work we do, including how we will make decisions regarding covid-19 vaccines," Marks and Hahn wrote.
The FDA has already said that it would want to see an efficacy of at least 50%, which means that any vaccine, to be considered, would need to reduce the risk of infection or serious disease by at least 50% relative to a placebo.
In a series of tweets from Dr. Peter Hotez, professor and dean of Tropical Medicine at Baylor School of Medicine, he noted earlier this month that "the USA involves poor or minor reviews."
"How can a poor or minor review be justified for something that would be injected into tens of millions, maybe hundreds of millions of Americans?" Hotez said.
In addition, he noted that mRNA technology, which is used in two of the most advanced vaccines in phase 3 trials - the Moderna vaccine and the Pfizer / BioNTech vaccine - is "a new technology that has never been licensed before.
We have no history or experience with these types of vaccines.
Even more reason for a full / comprehensive review. '
Hotez also mentions that in this highly politicized climate, there is a lack of trust in the government and federal agencies.
“We have seen how, in 2020, the White House has abused the US mechanism.
Remember the FDA revoked the EUA for hydroxychloroquine?
Neither is the White House or the Department of HHS, ”he tweeted.
The political connotation
There is also concern that the president is seeking to make a vaccine available for political reasons in the run-up to the November election.
President Trump has said multiple times that he believes a vaccine could be available by Election Day.
Without a doubt, the pace of medical innovation has moved faster than ever, with human vaccine trials beginning just 67 days after the virus was first identified.
The CDC recently told public health officials to prepare to distribute a possible vaccine in late October.
And FDA Commissioner Dr. Stephen Hahn said he would consider an emergency use authorization before phase 3 trials are completed.
OPINION |
Why Trump Should Care If He Gets A Rushed Vaccine
Pressure in the US for a vaccine before the election 1:04
Still, several government health officials have told CNN that the idea that a vaccine could be available to the general public by November 3 is unlikely.
“There is great concern about the kind of political expediency and when this date [October] was chosen… and just choosing this date, before the elections, fuels fears that the government is not being diligent enough to make sure that any vaccine is not only effective, but has few side effects, "said Dr. Ali Khan, dean of the School of Public Health at the University of Nebraska Medical Center, and former director of the Office of Health Preparedness Public at the CDC.
“So we are all optimistic that there are currently three vaccines in phase 3 trials, that maybe one of these vaccines is so great that you don't need to vaccinate 30,000 people to know it's going to work.
However, the concern is that if a full set of these so-called phase 3 trials is not done, the rare side effects will be missed, ”he told CNN earlier this month.
When a vaccine, or other medical product, is given to enough people, rare side effects can occur.
In 1976, the government launched a hastily produced vaccine about seven months after the Ford government believed a pandemic caused by a new strain of flu was imminent.
The pandemic never materialized, but 40 million people were vaccinated under a mandatory schedule.
Later, that vaccine was linked to a neurological disorder called Guillain-Barré syndrome, which can develop after an infection or, rarely, after vaccination with a live vaccine.
The link was never tested, but the program was stopped.
Furthermore, to demonstrate the efficacy of the vaccine, dozens of people in the placebo group would need to be infected, while very few infections, if any, would be seen in the vaccinated group of trial participants.
It may take weeks, if not months, to see that difference between the two populations.
Experts question the FDA's role against the 1:24 vaccine
Lack of trust
The public's lack of trust and doubts about vaccines are real.
A CNN poll in August showed that 40% of Americans do not want a vaccine when it is available, even if it is cheap and readily available.
Such low absorption of the vaccine could impair the country's ability to control the virus and return to normal.
If history is any indication, skepticism, if not outright mistrust, about an unapproved vaccine is nothing new.
In a study published in 2009, months after the United States declared a public health emergency due to the H1N1 flu and the World Health Organization declared it a pandemic, researchers explored the public's willingness to use a drug or vaccine with an emergency use authorization (not fully cleared by the FDA) by surveying a representative sample of more than 1,500 American adults.
They found that more than 77% of those surveyed would be moderately, very, or extremely concerned if they were offered an unapproved vaccine;
63% said they would not accept it.
They encourage minority participation in clinical trials 2:17
But there were also a few other key factors that would convince respondents that a vaccine licensed under an EUA was safe to use.
If the vaccine were administered by a public health professional, 55% of those surveyed say they would take it.
If it came with a newsletter, just over 57% of those surveyed said they would receive it.
And if it were administered by your own healthcare provider, that number shot up to 68%.
Transparency is key to gaining trust.
Health experts defend science
The heads of the country's health agencies - Alex Azar, from the United States Department of Health and Human Services;
Dr. Francis Collins of the National Institutes of Health;
Dr. Anthony Fauci, of the National Institute of Allergy and Infectious Diseases;
Dr. Stephen Hahn of the FDA and Dr. Robert Redfield of the CDC — have tried to assure Americans that policy will not influence when a vaccine becomes available.
Fauci has said that he believes a vaccine will likely be approaching the end of the year and that he would not be comfortable with making a vaccine widely available unless scientific evidence supports it.
I'm not a regulator.
I mean, I just do science.
It would report science accurately, and certainly if I saw interference, it would bother me a lot and say so, "Fauci told Jim Acosta on CNN's" The Situation Room. "
As for an emergency use authorization, "I would not feel comfortable with a vaccine unless a clinical trial clearly shows that it is safe and effective," Fauci said during an interview on NBC's "Today Show."
Dr. Luciana Borio, former FDA Acting Chief Scientific Officer, agrees that a vaccine must first be shown to be safe and effective.
But if a vaccine is shown to be safe and effective in adequate and well-controlled clinical trials, it should not be withheld until all strict licensing requirements for FDA approval are met, because some of the requirements cannot be generated quickly. .
"Safe and effective vaccines can save lives and help contain the pandemic," Borio tweeted.
"The EUA is the most appropriate regulatory mechanism to distribute vaccines that have been shown to be safe and effective in phase 3 randomized controlled trials, but do not yet meet all FDA clearance standards."
Moncef Slaoui, senior advisor to
Operation Warp Speed
, the Trump administration's effort to get a vaccine as soon as possible, said it would "be unethical" not to act quickly to launch a COVID-19 vaccine if it is shown to work.
"If we know that a vaccine is 70%, 80% or 90% effective, it would be unethical to retain it," Slaoui said during an interview with CNN on Friday.
Nine biopharmaceutical companies, including those most advanced in their vaccine testing programs, signed an unusual pledge to maintain "high ethical standards," suggesting that they will not seek premature government approval for COVID-19 vaccines.
They committed to "submit for emergency use approval or authorization only after demonstrating safety and efficacy through a Phase 3 clinical study, designed and conducted to meet the requirements of expert regulatory authorities such as the FDA."
Ethical pact of biopharmaceuticals to obtain safe vaccine 1:27
In fact, later that day, AstraZeneca, one of the signatories to the pledge, said that it had halted its trials globally due to an unexplained illness in a volunteer in the UK.
The pharmacist called the pause "a routine action."
“In large trials, diseases will happen by chance, but they need to be independently reviewed to verify this carefully.
We are working to expedite the single event review to minimize any potential impact on the trial schedule, "AstraZeneca said, in a statement sent to CNN.
According to FDA guidance, any vaccine, whether emergency licensed or approved, must prevent disease or at least decrease severity by at least 50%.
Despite all the intrigue, it may be worth going back to the original criteria for an EUA, in particular the stipulation that it will only be awarded when "there are no suitable, approved and available alternatives."
While most people understandably do not want to hear it, there is a reasonable alternative, which has worked well in many parts of the world, and that is to respect basic public health measures: wear a mask, maintain physical distance, have good hand hygiene practices and stay away from large crowds, especially indoors.
Following those rules will significantly reduce the likelihood of people getting sick and slow down the transmission of the virus.
It will also give us more time to make sure the evidence supporting the vaccine is fully defined.
- CNN's Jen Christensen, Shelby Lin Erdman and Nadia Kounang contributed to this report.
Coronavirus Vaccine