"Now we cannot choose a vaccine," says expert 6:17
(KHN) -
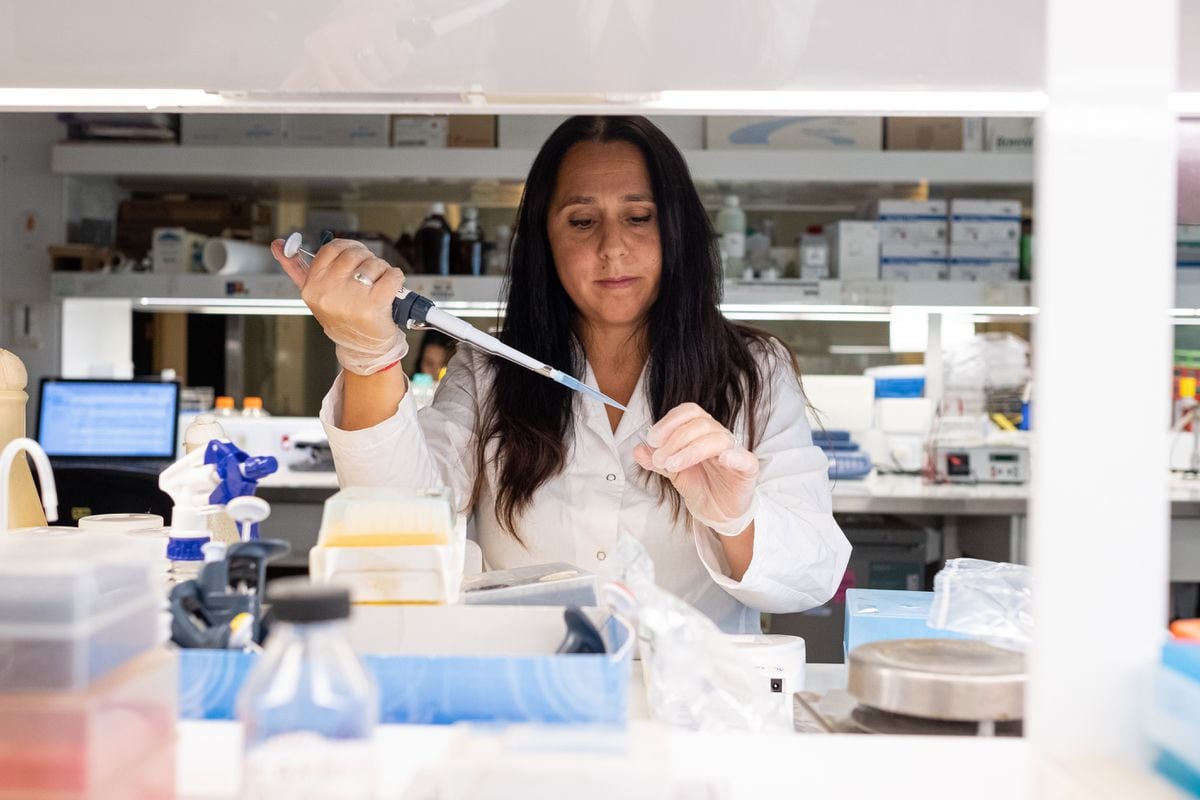
Dr. Andrew Carroll, a GP in Chandler, Arizona, wants to help his patients get vaccinated against COVID-19.
That's why it paid more than $ 4,000 for an eBay ultra-low-temperature freezer needed to store the Pfizer vaccine.
But he's not sure if he has a chance to use it, given that health officials have so far not said when he will be vaccinated in private doctors' offices.
"I'm very angry," Carroll said.
Not only do physicians have trouble vaccinating patients, but many community physicians and medical staff who are not employed by hospitals or health systems also report mixed results when vaccinating.
Some have received their vaccinations, but others are still waiting, although healthcare workers who provide direct patient care are in the top priority group of the US Centers for Disease Control and Prevention.
Many of these doctors say they don't know when (or if) they will receive doses for their patients, which will soon become a bigger problem as states try to vaccinate more people.
advertising
"The reason that is important is because patients trust their doctors when it comes to the vaccine," said Carroll, who has complained on social media that his county has not yet posted plans on how to incorporate the primary care physicians to the circuit.
China's covid-19 vaccines: what we know about Sinopharm, CanSino and Sinovac
How to face the phobia of water before getting vaccinated?
2:05
Doctors seek to obtain covid vaccines for their patients
Together, county doctors could vaccinate thousands of patients a day, he said, and could attract some who would otherwise hesitate if they had to go to a large hospital, a fairground or another central location.
Their concern arises because, at the national level, the launch of the vaccine has had a slower start than expected, far behind the initial goal of administering 20 million doses before the new year.
But Dr. Jen Brull, a family practice physician in Plainville, Kansas, said her rural area has made good progress in the first phase of vaccinations, and acknowledges the close working relationships formed long before the pandemic.
This fall, before the doses were available, the local hospital, the Health Department, and medical offices coordinated a registration list for medical workers who wanted the vaccine.
So when their county, with a population of 5,000, received its first 70 doses, they were ready to go.
Another 80 doses arrived a week later.
"We will be able to vaccinate almost everyone in the county who wanted it related to health care," Brull said recently.
Vaccination gaps
But that is not the case everywhere.
Dr. Jason Goldman, a family physician in Coral Gables, Florida, said he was able to get vaccinated at a local hospital that received most of the vaccines in his county and oversaw the distribution.
In the weeks that followed, however, he said that several of his front-line staff still "don't have access to the vaccine."
Also, "a lot" of patients are calling his office because Florida has relaxed distribution guidelines to include anyone 65 and older, Goldman said, asking when they can get the vaccine.
He has asked officials to distribute the vaccines through his practice, but has received no response.
Patients "are frustrated because they don't have clear answers and because they are not giving me clear answers to provide," he said.
"We have no choice but to direct them to the health department and some of the hospital systems."
Another point of concern for Goldman, who served as the liaison between the American Academy of Family Physicians and the panel of experts that develops the CDC's distribution guidelines, is the tremendous variation in how those recommendations are implemented across states.
Azar: States should expand covid-19 vaccination to all vulnerable people
Can companies force their employees to get vaccinated?
1:30
The phases of the coronavirus vaccine
The CDC recommends several phases, with frontline healthcare workers and nursing home residents and staff in the initial pool.
Then, in the second part of that phase, come the seniors over 75 and non-healthcare frontline workers, which could include first responders, teachers, and other designated essential workers.
States have the flexibility to design their own implementation program and priority groups.
Florida, for example, offers doses to anyone 65 and older.
In some counties, seniors were told that vaccines were available on a first-come, first-served basis, a move that has resulted in long lines.
"To say right now [that people over 65 should be vaccinated], when not even all healthcare workers have been adequately vaccinated, is to deny the phase," Goldman said.
'There has to be a national standard.
We have those guidelines.
We need to get a little supervision.
On Thursday, the American Hospital Association echoed that concern in a letter to the Secretary of Health and Human Services (HHS), Alex Azar.
Hospitals, along with health departments and large pharmacy chains, are making most of the vaccines.
In a call for additional coordination by federal officials, the letter outlined what it would take to reach the goal of vaccinating 75% of Americans by the end of May: 1.8 million vaccines per day.
Noting that there are 64 different implementation plans from states, cities and other jurisdictions, the letter asked whether HHS "assessed whether these plans, taken together, are capable of achieving this level of vaccination."
Making Your Vaccine Plan Work: Private Doctors Are Key
The lack of direct national strategy or support means that each county is essentially alone, and success or failure is affected by available resources and the expertise of local officials.
Most state and local health departments are underfunded and under intense pressure due to the growing pandemic.
However, the success of vaccination efforts depends on planning, preparation, and clear communication.
In Lorain County, Ohio, with a population of 310,000, local officials began practicing in October, said Mark Adams, deputy health commissioner.
They established mass vaccination clinics for influenza to study what would be needed for a vaccination effort against COVID-19.
How many employees?
What would the traffic flow be like?
Can patients be kept at a distance of two meters?
"That gave us an idea of what is good, what is bad and what needs to change," said Adams, who has had prior experience coordinating mass vaccination efforts at the county level.
So when the county received its first shipment of 500 doses on December 21, Adams had his plan in place.
He called the fire chiefs to invite all the emergency medical technicians and affiliated personnel to an ad hoc vaccination center set up in a large entertainment venue staffed by his health department.
Upon arrival, people were greeted at the door and directed to separate "lanes" where they would receive their vaccinations, then to a monitoring area where they could wait 15 minutes to make sure they didn't have a reaction.
Just after Christmas, another 400 doses arrived and the makeshift clinic reopened.
This time, the doses were for community doctors, dentists and other physicians, 600 of whom had previously enrolled.
(Hospital workers, staff, and nursing home residents are getting their vaccinations through their own institutions.)
As they move into the next phase, beneficiaries include residents over 80, people with developmental disorders and school staff, the challenges will grow, he said.
The county plans a multi-pronged approach to notifying people when it is their turn, including using a website, local media, churches, other organizations, and word of mouth.
Adams shares the concerns of medical providers across the country: You receive just two days' notice of how many doses you are going to receive, and at the current rate of 400 or 500 doses per week, it will be a while before most residents in the county has the opportunity to receive a vaccine, including the approximately 33,000 people 65 and older.
With 10 nurses, his clinic can inject around 1,200 people a day.
But many other healthcare professionals have volunteered to give you the injections if you get more doses.
"If I had three clinics, five days a week, I could do 15,000 shots a week," Adams said.
"With all the volunteers, I could do almost six clinics, or 30,000 a week."
Still, for those in the last public group, those 18 and older with no underlying medical conditions, "it could be summer," Adams said.
- KHN (Kaiser Health News) is a non-profit news service that covers health topics.
It is an editorially independent program of KFF (Kaiser Family Foundation) that is not affiliated with Kaiser Permanente.
Coronavirus Vaccine