USA would achieve herd immunity in 10 months 1:33
(CNN) -
You may be among the more than 27 million people in the United States who were infected with Covid-19, and you have many questions about vaccines, emerging variants or the risk of re-infection.
"We are still learning after a year of pandemic," Dr. Becky Smith, medical director of infection prevention and control and infectious disease specialist at Duke University Hospital, told CNN in an email.
However, there are some answers to questions that, according to doctors, those people who have survived COVID-19 should know.
What is the risk of reinfection?
The risk of reinfection "appears to be quite low" and the Centers for Disease Control and Prevention (CDC, for its acronym in English) "state that the risk of reinfection is 'low' within the first 90 days after having infected with covid, "Smith said.
Although rare, there is a risk.
"Based on what we know of similar viruses, some reinfections are expected," the CDC notes on its website.
"The risk of reinfection remains low, but we must be on the lookout for new variants," Dr. Antonio Crespo, medical director of infectious diseases at the Orlando Health Medical Group Infectious Disease, told CNN.
advertising
The new coronavirus that causes covid-19 has changed over time, as all viruses do, and variants of the virus have emerged through these mutations.
READ: Why do viruses mutate?
This is how scientists study the variations of the coronavirus
Scientists are not surprised to see the coronavirus change and evolve.
After all, that's what viruses do.
And with so much rampant spread in the United States and other parts of the world, the virus has many opportunities to do just that.
What about the new variants?
So far, three variants circulating around the world have been identified and received much attention: variant B.1,1.7 was first identified in the UK, variant B.1,351 was first identified in South Africa, and variant B.1,1.7. variant P.1 was detected for the first time in Brazil.
Globally circulating variants of the coronavirus are projected to become more dominant in the United States in the spring, said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, during a press conference at the White House. last week.
USA exceeds 27 million cases of covid-19 0:51
In the same briefing, CDC Director Dr. Rochelle Walensky said that all COVID-19 cases in the United States should now be treated as if they were caused by one of the newly identified coronavirus variants.
Another reason why the risk of reinfection remains a mystery is that it is unclear how long antibodies to covid-19 can last in the body.
How long will my antibodies last?
Antibodies are proteins your body makes shortly after you are infected.
They help fight infection and can protect you from getting the disease again.
"What we know is that when someone is infected with COVID-19, they get antibodies that can last," said Crespo.
"But now the new scientific knowledge that is emerging is that some of the coronavirus variants could evade antibodies and could be potentially infectious for someone who has already been infected with a known variant of covid-19," he explained.
Smith said that in a large study of more than 12,000 healthcare workers at Oxford University hospitals in the UK, very few with antibodies were infected a second time over a six-month period.
That study, published in the
New England Journal of Medicine
in December, suggests that antibodies are associated with "a substantially lower risk of reinfection."
"Those who developed a reinfection had had asymptomatic infections," Smith said in his email.
Smith added that anecdotal evidence from his hospital's experience in managing healthcare workers infected with COVID-19 suggests that the antibodies likely protect against reinfection.
"To date, approximately 0.5% of healthcare workers have experienced reinfection events, although we recognize that COVID antibodies have not been routinely verified as in the Oxford study," said Smith, who was not involved. in the study.
Recent Findings
People who have been infected with COVID-19 may be protected from contracting it again for at least five months, according to a new study led by Public Health Great Britain.
The study, which has not yet been peer-reviewed, found that having had a previous infection was associated with an 83% lower risk of reinfection compared to people who had never been infected.
However, the researchers cautioned that the protection was not absolute, meaning that some people contract the virus again, and that it was not clear how long immunity lasts.
It is also possible that those with some degree of immunity can carry the virus in their nose or throat and, therefore, transmit it to other people.
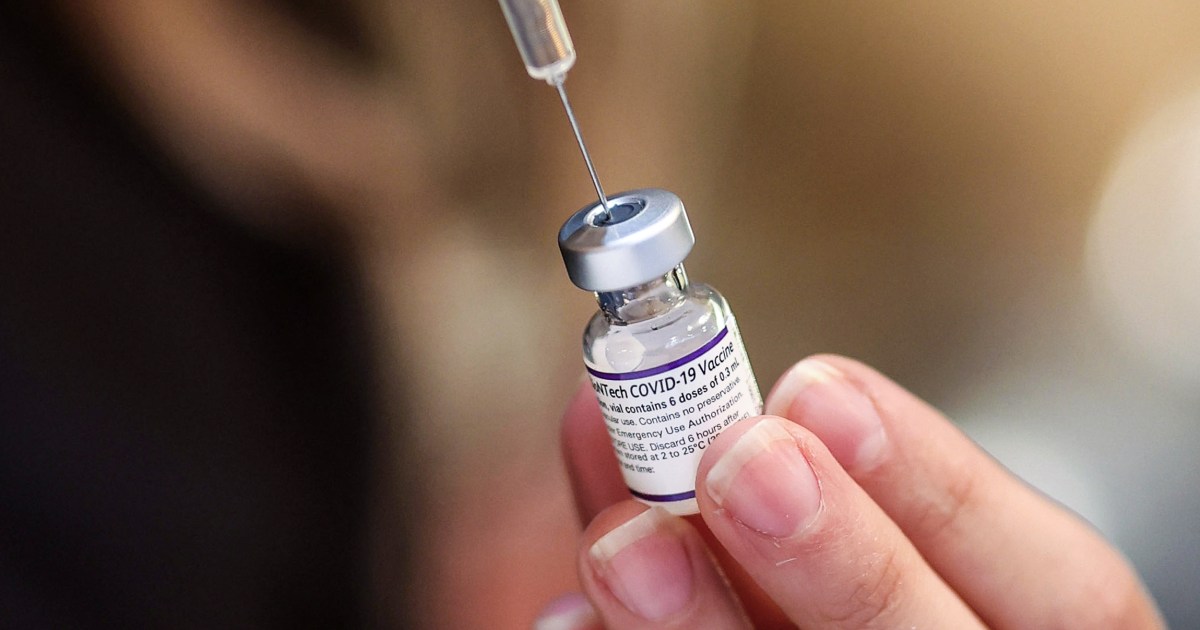
Do I need to get vaccinated if I have covid-19?
Doctors and health officials encourage people who have had COVID-19 to get vaccinated anyway.
Data from advanced-stage clinical trials suggest that the vaccines are safe and help protect people who have already been infected with COVID-19 from reinfection.
This, regardless of whether your previous case was mild or severe.
"Even if someone had a natural COVID-19, my recommendation is to get vaccinated as soon as the vaccine is available to the person," Smith said.
US pharmacies begin vaccination on February 11 1:12
“It is very clear that the two available vaccines offer a high level of protection as measured by neutralizing antibody titers.
This may be particularly important for people who had an asymptomatic or mild infection, "he said.
"Having a higher level of antibody titers to begin with will protect you for longer," he explained.
Smith added that the Pfizer / BioNTech and Moderna vaccines, licensed for emergency use in the United States, appear to provide some protection against emerging variants of the coronavirus circulating the world.
"We are not sure whether natural immunity will protect people from becoming infected with the new strains," Smith said.
Should I go get vaccinated if I'm sick now?
However, a person who is currently sick with Covid-19 must wait to receive the vaccine after their symptoms have disappeared and they can come out of isolation.
There is no minimum time recommendation between infection and vaccination.
Also, there is no safety data on people who have received convalescent plasma or antibody therapy to treat a COVID-19 infection.
Since reinfection appears to be rare within 90 days of initial infection, the CDC recommends as a precaution that a person wait at least 90 days.
READ: 10 things you should do and avoid before and after receiving the covid-19 vaccine
There is no data to show that the vaccine would protect a person who has been recently exposed.
A person is not fully protected until a week or two after receiving the second dose of the vaccine.
Do I need both doses of the vaccine?
The Pfizer / BioNTech and Moderna vaccines licensed for emergency use in the United States are administered in two doses, 21 and 28 days apart respectively.
It is currently recommended that people stick to that vaccination schedule until more research is conducted and health officials make another recommendation.
The reason why you don't have to wait to get vaccinated 1:49
"The concept of giving a single booster vaccine to those who have had a natural infection has been put forward as a way of preserving the limited supply of vaccines and making them available to those who never developed covid infection," Smith said.
New evidence
A pre-printed document, which was posted on the online server medrxiv.org on Monday, shows some evidence that after receiving a single injection of the covid-19 vaccine, people who had previously been infected with the virus tended to have antibody levels that were equal to or higher than those of people who had received both doses but had never been previously infected.
The study does not specify which vaccines the participants received.
"Logically, people who have had a COVID infection are likely to start with a baseline of some detectable neutralizing antibody, so they don't start from scratch like people who never had COVID," Smith said.
"However, the amount of neutralizing antibodies decreases over time, so this needs to be carefully studied before implementing it," he said.
"We would need data to determine the optimal timing of the boost from natural infection and whether the duration of protection is equivalent to the protection you get with two doses of the vaccine," he explained.
Smith added that variants of the coronavirus would also remain a risk.
'We are also not sure about variant strains and how well antibodies developed from a natural infection protect a person against a new strain.
The vaccines have been tested and provide protection based on limited data, ”Smith said.
"Ultimately, this approach would require patients to be tested for antibodies prior to vaccination and this may not be readily available to everyone," he added.
Could you continue to experience long-term effects from covid-19?
Many survivors of Covid-19 can experience symptoms for weeks or months.
«Patients may experience persistent severe fatigue, headaches, mental confusion, mild cognitive impairment / difficulty thinking or concentrating, joint pains, coughing, shortness of breath, intermittent fevers and alterations in taste and smell, among others symptoms, ”Smith said.
"These persistent symptoms can last up to 12 weeks and many say that symptoms increase and decrease or come and go during that time," he explained.
"Some people have mild symptoms and recover quickly and have no major problems.
One of the side effects that we have seen very frequently is chronic fatigue, ”said Crespo.
"It seems that, in patients with COVID-19, it is one of the common symptoms that can persist for several months," he added.
"Also, if patients have had significant lung involvement with severe pneumonia, they may have a hard time recovering from persistent shortness of breath, coughing, and easy tiredness," he said.
Crespo added that even if you have lingering effects, it is important to get the vaccine when it is your turn.
"They should get the vaccine," he said.
"I don't see that having long-term effects has a particular effect on the response to the vaccine," he explained.
CNN's Zamira Rahim, Maggie Fox, Jen Christensen, Amanda Sealy, and Michael Nedelman contributed to this report.
Coronavirus Vaccine