Covid-19, the third leading cause of deaths in the US in 2021 1:26
(CNN) --
When you think of post-traumatic stress disorder (PTSD), your mind may think of a movie about war.
It's a quiet day at a base camp when suddenly the enemy launches an attack.
The main character struggles to respond to incoming fire, making quick decisions about how to respond to danger that is largely out of his control.
In many ways, it's a lot like the experiences of family members of patients who are in an intensive care unit for Covid-19, said Dr. Timothy Amass, an assistant professor of medicine at the University of Colorado School of Medicine.
Family members very often see an abrupt change in circumstances, have to make difficult decisions quickly and feel a loss of control, he said.
And they often come away from the experience with symptoms of anxiety, depression and PTSD, according to a new study published Monday in JAMA Internal Medicine.
"When you put that in a hospital, the sudden change in health status is mom or dad was healthy yesterday and now they're in the ICU on life support," said Amass, the study's first author.
advertising
Having a loved one in an ICU has always been an inherently stressful and often traumatic process, but the Covid-19 pandemic has pushed researchers to take an even closer look at the impacts, he said.
Amass and her team surveyed family members of COVID patients in ICUs in the months after they were admitted to intensive care units at 12 US hospitals.
Many of these people had limited visits and contact with the patient.
The study found that of the families who responded to the survey, 201 of 316 (about 63%) had significant symptoms of post-traumatic stress disorder.
There's a possibility that those who experienced the most emotional distress responded to a greater extent, and that the findings could exaggerate PTSD symptoms as a result, said Dr. Murray Stein, vice chair for clinical research in the School's Department of Psychiatry. of Medicine at the University of California San Diego.
Stein was not involved in the study.
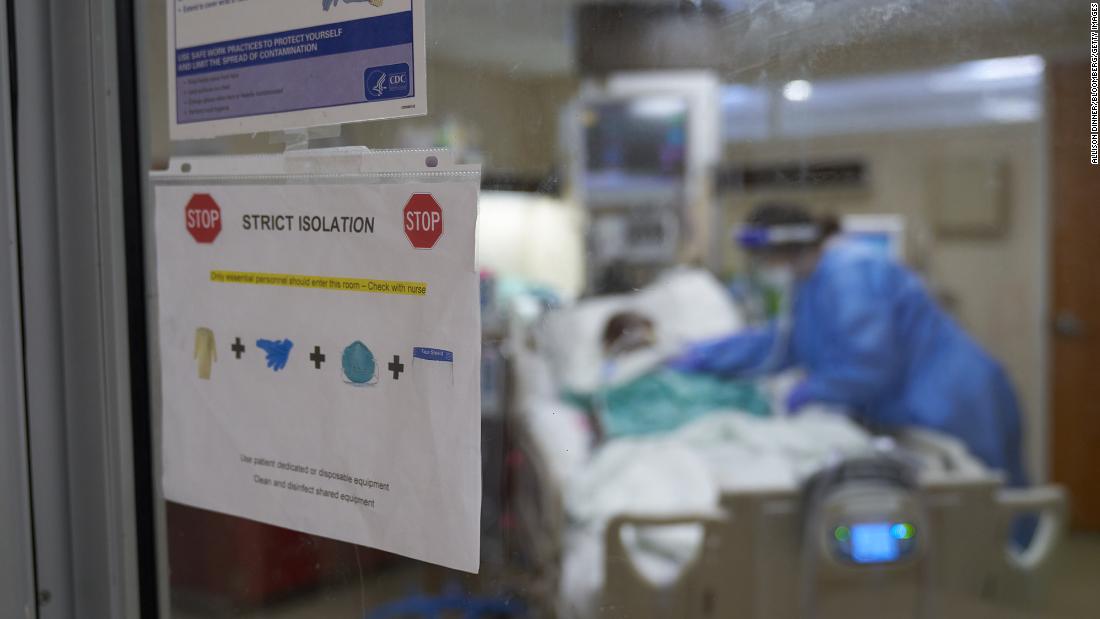
This hospital changed the severity of covid-19 isolation for the love of families
Especially early in the pandemic, many families struggled with not having as much access to visitation and communication with their loved ones who were hospitalized with Covid-19, said Dr. Timothy Amass, an assistant professor of medicine at the University School of Medicine. from Colorado. (Credit: Allison Dinner/Bloomberg via Getty Images)
"All of this said, even if the rates are only half of what this study found, they are still alarmingly high and point to a need for emotional support," added Stein, who is also a distinguished professor of psychiatry and public health at UC .
San Diego.
Covid-19 is not yet like the flu, experts warn
What you need to know about the covid-19 breath test 2:15
An approach for families with covid-19 patients
The health care community can take two important steps to help improve the experience for families: pay attention to their risk factors and do more to empower them, Amass said.
"What the literature really suggests is that the more you engage someone at the bedside, the more empowered they feel to express both their needs and those of their loved ones," she said.
In addition to the survey, the study also used narrative interviews to get more details about what made a difference for families.
Some may have experienced staff going the extra mile to make them feel connected and involved even when they couldn't be there.
"What made it easier were the video consultations, the video calls and the daily updates. I called and talked to the nurses every day, I talked to the doctor," said a family member of a COVID patient hospitalized in an ICU, according to the study. .
But other survey participants felt the communication they received was limited and reported feeling powerless and fearful.
"They called us and said, 'Do you want us to take it offline?'
... I said, how did he go from going home to being unplugged?... They say his mouth was moving and his eyes were moving, but they said she was dead...so they went ahead and unplugged anyway," another relative of another patient said.
Especially at the start of the pandemic, hospitals were overwhelmed and staff members were working long hours to provide the best possible care.
Amass said it's often small acts of kindness that families need to feel the sense of involvement and care for their loved one that they need, like asking for a photo that hospital staff can hang to make the patient feel happier.
"Even that small act of compassion from the health care team toward the family can really have a really powerful impact on those family members and their risk of developing these (post-traumatic stress) symptoms," Amass said.
More research may be needed to understand how health care providers can best interact with families after an ICU stay, but this latest study suggests stronger services are needed, Stein said.
"The scores on these surveys were so high that I would recommend providers actively clinically screen these family members for depression, anxiety and PTSD so they can receive therapy," Amass said.
Covid-19