What is the transplant impossible to perform?
1:42
(CNN) --
What if doctors could simply print out a kidney, using cells from the patient, instead of having to find a matched donor and hope that the patient's body wouldn't reject the transplanted kidney?
The soonest that could happen is within a decade, thanks to 3D bioprinting of organs, according to Jennifer Lewis, a professor at the Wyss Institute for Biologically Inspired Engineering at Harvard University.
Organ bioprinting is the use of 3D printing technologies to assemble multiple cell types, growth factors, and biomaterials in a layer-by-layer manner to produce bioartificial organs that ideally mimic their natural counterparts, according to a 2019 study.
This type of regenerative medicine is under development, and the driver of this innovation is "real human need," Lewis said.
In the United States, there are 106,075 men, women and children on the national organ transplant waiting list as of June 10, according to the Health Resources and Services Administration (HRSA).
However, living donors only contribute an average of 6,000 organs a year, and there are about 8,000 deceased donors a year who contribute an average of 3.5 organs each.
A 95-year-old man just became the oldest organ donor in US history.
The cause of this discrepancy is "a combination of people experiencing catastrophic health events, but their organs aren't of high enough quality to donate, or they're not on the organ donor list to begin with, and the fact that it's actually very difficult to find a good match" so that the patient's body doesn't reject the transplanted organ, Lewis said.
And while living donors are an option, "operating on someone who doesn't need it" is a big risk, said Dr. Anthony Atala, director of the Wake Forest Institute for Regenerative Medicine.
"So living related donors are often not the preferred option, because then you're taking an organ from someone else who might need it, especially now that we're getting older longer."
advertising
Atala and his colleagues were responsible for manually growing human bladders in a laboratory in 2006, and implanting a complicated internal organ in people for the first time, saving the lives of three children who had the bladders implanted.
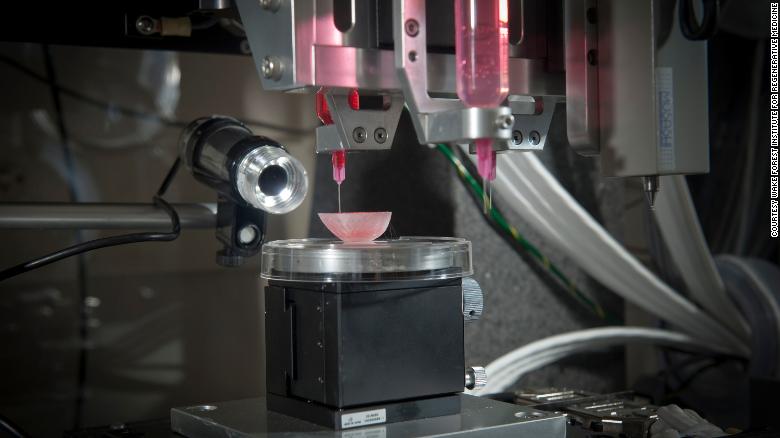
A bladder scaffold is seeded with cells at the Wake Forest Institute for Regenerative Medicine.
Every day 17 people die waiting for an organ transplant, according to the Health Resources and Services Administration.
And every nine minutes another person is added to the waiting list, according to the agency.
More than 90% of people on the transplant list in 2021 needed a kidney.
"About a million people around the world need a kidney. So they have end-stage kidney failure and they have to go on dialysis," Lewis said.
"Once you go on dialysis, you have essentially five years to live, and every year, your mortality rate increases by 15%. Dialysis is very hard on the body. So this is really motivating to take on this great challenge of print organs".
"Antihypertensives are not in short supply. Everyone who needs them can get them," said Martine Rothblatt, CEO and president of United Therapeutics, at the Life Itself conference, a health and wellness event presented in partnership with CNN.
United Therapeutics is one of the sponsors of the conference.
"There is no practical reason why someone who needs a kidney, or a lung, a heart, a liver, can't get it," he added.
"We are using technology to solve this problem."
How organ printing works
To start the process of bioprinting an organ, doctors often start with the patient's own cells.
They take a small needle biopsy of an organ or perform a minimally invasive surgical procedure that removes a small piece of tissue, "less than half the size of a postage stamp," Atala said.
"By taking this little piece of tissue, we can separate the cells (and) grow and expand them outside the
body."
This growth occurs inside a sterile incubator or bioreactor, a pressurized stainless steel container that helps keep cells fed with nutrients, called "media," that doctors give them every 24 hours, since cells have their own metabolism, Lewis said.
Each cell type has a different medium, and the incubator or bioreactor acts as an oven-like device that mimics the internal temperature and oxygenation of the human body, Atala said.
"Then we mix it with this gel, which is like glue," Atala said.
"Every organ in the body has the cells and the glue that holds it together. Basically, that's also called the 'extracellular matrix.'"
This glue is Atala's nickname for bioink, a printable mixture of living cells, water-rich molecules called hydrogels, and the media and growth factors that help cells continue to proliferate and differentiate, Lewis said.
Hydrogels mimic the extracellular matrix of the human body, which contains substances such as proteins, collagen, and hyaluronic acid.
The non-cellular sample part of the glue can be made in a lab and "is going to have the same properties as the tissue you're trying to replace," Atala said.
The biomaterials that are typically used have to be nontoxic, biodegradable and biocompatible to avoid a negative immune response, Lewis said.
Collagen and gelatin are two of the most widely used biomaterials for tissue or organ bioprinting.
Baby receives first heart and thymus transplant, which could eliminate the need for dangerous medication for life
The printing process
From there, doctors load each bioink, depending on the number of cell types they want to print, into a printing chamber, "using a head and nozzle to extrude an ink and build the material layer by layer," explains Lewis. .
Creating fabrics with personalized properties is possible because the printers are programmed with the patient's image data from X-rays or scans, Atala explained.
"With a color printer you have several different cartridges, and each cartridge prints a different color, and you get the (final) color," Atala added.
Bioprinting is the same thing, only cells are used instead of traditional inks.
The length of the printing process depends on several factors, such as the organ or tissue being printed, the accuracy of the resolution, and the number of printheads required, Lewis explains.
But it usually lasts a few to several hours.
The time from biopsy to implantation is about four to six weeks, Atala said.
A 3D printer seeds different types of cells on a kidney scaffold at the Wake Forest Institute for Regenerative Medicine.
The ultimate challenge is "getting the organs to really work the way they should," so getting that "is the holy grail," Lewis said.
"Just like taking an organ from a donor, you have to immediately put it in a bioreactor and start perfusing it or the cells will die," he added.
To perfuse an organ is to supply fluid, usually blood or a blood substitute, by circulating it through blood vessels or other channels.
Depending on the complexity of the organ, it is sometimes necessary to further mature the tissue in a bioreactor or further boost connections, Lewis said.
"There are a number of plumbing issues and challenges that need to be done to get that printed organ to actually function like a human organ would in vivo (i.e. in the body). And honestly, this hasn't been fully resolved yet." ".
Once a bioprinted organ is implanted in a patient, it will naturally degrade over time, which is fine because that's how it's designed to work.
"You're probably wondering, 'Well, what about the fabric? Will it fall apart? Not really,'" says Atala.
"These glues dissolve, and the cells feel that the bridge is giving way; they feel that they no longer have a firm foundation. So the cells do what they do in their own body, which is create their own bridge and create their own glue." .
pending challenges
Atala and Lewis are conservative in their estimates of the number of years remaining before fully functioning bioprinted organs can be implanted in humans.
"The field is moving fast, but I think we're talking over a decade, even with all the tremendous progress that's been made," Lewis said.
Man who received first genetically modified pig heart transplant dies
"I learned many years ago to never predict because you are always wrong," Atala said.
"There are so many factors in terms of manufacturing and (US Food and Drug Administration regulation). In the end, our interest, of course, is to make sure the technologies are safe for the patient above all".
When organ bioprinting becomes an available option, affordability for patients and their caregivers should not be an issue.
They will be "affordable, no doubt," Atala said.
"The costs associated with organ failure are very high. Keeping a patient on dialysis costs more than a quarter of a million dollars a year. So it is much cheaper to create an organ that can be implanted in the patient."
The median cost of a kidney transplant was $442,500 in 2020, according to research published by the American Society of Nephrology, while 3D printers sell for anywhere from a few thousand dollars to more than $100,000, depending on their size. complexity.
However, even if low-cost printers exist, the most expensive parts of bioprinting can include maintaining cell banks for patients, culturing them, and safely handling biological materials, according to Lewis.
Some of the main costs of organ transplants today are "removal of the donor organ, transportation costs and, of course, the surgery that the recipient undergoes, as well as all the care and follow-up," he said. Lewis.
"Some of that cost would still apply, even if it was bioprinting."
3D printingTransplants