Immunotherapy has revolutionized the treatment of cancers but is still booming.
By
“
boosting
”
the immune system, this approach allows the recruitment of immune cells to the tumor to prevent it from developing and gradually make it disappear, until complete remission.
However, for reasons so far unknown, many patients are still resistant to it.
Nivolumab, for example, used to treat melanoma, kidney or lung cancer, is only effective for one in five patients.
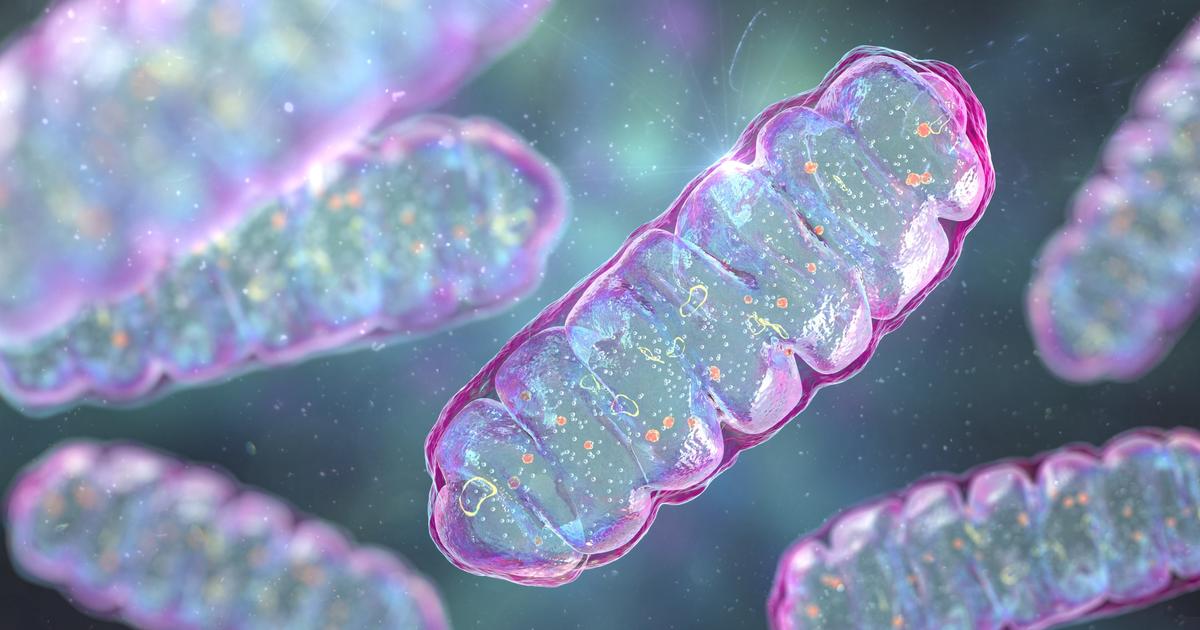
And according to a new study, one of the explanations for this resistance is found in our mitochondria, these miniature “powerhouses” which produce ATP, the energy substrate that all our cells need.
In theory, mitochondria are energy sinks, including for cancer cells which have very high needs for their own growth.
However, around half of human cancers have mutations in mitochondrial DNA that block the activity of mitochondria.
The tumor cells then draw their resources from an alternative pathway, glycolysis, which is between 10 and 18 less efficient.
A flaw ?
Not really.
This trick allows cancer cells to escape the other major mode of action of mitochondria, that of inducing cell death.
However, in a new study published in
Nature Cancer
, researchers found that these mitochondrial DNA mutations also make cancers much more sensitive to immunotherapy treatments.
“
This is a major discovery because it opens up the possibility of predicting which patients would be more receptive to these heavy treatments ,
”
underlines Laurent Chatre, researcher at the CNRS, specialist in mitochondria and stress.
Also read: Stimulate immunity to treat cancer
Mutations that modulate immunity
The particularity of mitochondria is that they have their own DNA, independent of that of our cells.
It is called mitochondrial DNA or mtDNA.
Previous studies have shown that 50% of human cancers are characterized by mutations in this mtDNA.
A majority of them are located more specifically in a protein structure, “complex I”, involved in the production of ATP by the mitochondria.
In melanoma, up to 20% of mutations occur at this protein site.
“
ATP molecules are produced at the inner membrane of mitochondria by a mechanism involving five protein complexes, named I to V. They form what is called the mitochondrial respiratory chain.
When these proteins are mutated, their functioning is altered so that the mitochondria stop producing ATP ,
”
explains Dr. Chatre.
By bypassing this mitochondrial mechanism, cancer cells deprive themselves of an important source of energy but thus escape the ability of mitochondria to cause cell death.
However, the precise effect of these mutations on cancer cells was still unknown.
In this study, scientists were specifically interested in complex I mutations in melanoma.
To do this, they used tumor cells from a mouse melanoma, and introduced mtDNA mutations at the level of complex I into these cells in order to “imitate” those found in human melanoma. .
Then they reintroduced the modified cells into the mice.
They then found that tumors carrying mutations had undergone significant remodeling of immune cell activity in the tumor environment.
“
This inflammatory signature was, however, not observed in tumors which did not carry mtDNA mutations ,
”
underlines Clara Nahmias, CNRS research director at Gustave-Roussy hospital and founder of the PrOlific association.
“
This is an important result because it is from this that the authors hypothesized that these mtDNA mutations could play a crucial role in the response to immunotherapies
,”
insists the researcher.
Read the fileCancer, the hope of overcoming the disease
A response that is at least times more effective
Without much expectation, the scientists took on a crazy challenge.
They attempted to compare the response to nivolumab of diseased mice that did or did not carry these mutations in the mtDNA.
Result: nivolumab was found to be effective only against tumors carrying these mutations.
To find out if they found these results in humans, they sequenced mtDNA in tumor samples from a cohort of 70 patients with metastatic melanoma treated with nivolumab.
They then realized that patients carrying a large number of complex I mutations (more than 50% genetic variants) had responded 2.6 times better to treatment than other patients.
This response could be explained by the presence of stress factors in tumor cells, precisely because of mtDNA mutations.
“
When complex I proteins
are mutated, they malfunction and the mitochondria begin to produce
reactive oxygen species
which increase stress in the mitochondria and, therefore, in cancer cells.
They thus become more sensitive to immunotherapy treatments, in this case nivolumab ,
”
explains Laurent Chatre.
Also readCancer: immunotherapy now in pole position?
Towards precision medicine
Before this study, researchers did not suspect that mutated, therefore “sleeping,” mitochondria had a major influence on the resistance behavior of cancer cells.
Thus, this work has a potentially enormous impact because it opens a new era in personalized cancer treatment.
“
This discovery will probably be revolutionary in the fields of immunotherapies in the sense that we will now be able to target patients likely to respond better to these innovative treatments ,
”
believes Clara Nahmias.
Concretely, the authors suggest carrying out targeted sequencing on tumor samples usually taken to make the diagnosis of cancer.
This would make it possible to identify patients whose tumors carry numerous mutations in mtDNA and who are therefore more likely to benefit from immunotherapy.
“
We could start by looking for the famous complex
I mutations. But it is very likely that other mutations have this same effect ,
”
specifies Dr. Chatre.
They still remain to be discovered.