More bad news for AstraZeneca.
Now, his vaccine, after correction, would only be 76% effective against Covid-19.
This is three points lower than the rate which was initially announced, based on its clinical trial conducted in the United States.
But what does this number really mean?
Many of you have heard people around you or those not so close to compare the different vaccines.
It's the famous "Personally, I would prefer this one, it's the best!"
A reflection that it is very quickly tempting to expose, as the publications of pharmaceutical laboratories have been watched, relayed and commented on since the start of the health crisis.
What if things, once again, were a little more complex than they seem?
Many specialists agree to say it: it is perilous to launch out in the comparison of the various rates of effectiveness of the vaccines.
If the French currently do not have the ability to freely choose which potion is administered, this could happen someday.
So you might as well have all the parameters in mind.
Dive into the method of calculating these efficiency rates.
Or “efficacy rates”, as the Americans say.
What does this efficiency rate mean?
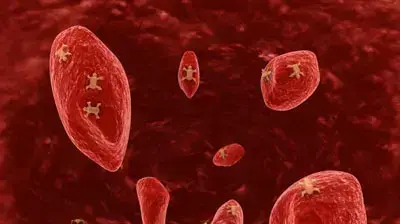
The efficacy rate of a vaccine measures the reduction in the risk of being infected with Covid-19 after having been vaccinated.
To fully understand the concept, it is necessary to detail (simply) the way in which this rate is calculated.
To take his example, Pfizer has found nearly 43,500 people around the world for its clinical trial.
This large sample was divided into two groups.
In the first, the volunteers were injected with two doses of the vaccine.
In the second, two doses of placebo (a product with no effect).
All these little people were then released into the wild for several weeks.
The researchers counted the number of contaminated candidates in each of the groups.
A total of 170 candidates were infected during the clinical trial and the efficacy rate was calculated according to their distribution: among them, 162 cases of contamination were identified in the placebo group, i.e. a little over 95 % sick people.
Against only 8 in the vaccinated group.
The clinical trial therefore shows that the Pfizer vaccine reduces the risk of being infected with the virus by 95% after vaccination.
The laboratory can then send its press release with great fanfare.
Why are the rates not comparable?
All pharmaceutical companies have used this methodology.
Nothing therefore prevents a priori from being able to compare them.
Except that its implementation has varied widely, from one lab to another.
A phenomenon further amplified in the case of Covid-19 by the scale of the crisis, and especially by the need to find an effective vaccine as quickly as possible.
"Faced with the global emergency, it immediately became apparent that we could not develop a vaccine in a conventional way, because this development would take years," details the Pfizer laboratory with the Parisian.
Conventionally, we proceed sequentially, each step does not start until after the end of the previous one.
In this case, given the urgency, we decided to launch several steps at the same time.
In other words, the labs overlapped the different phases of their clinical trials.
Dialogue has certainly been constant between the laboratories and the authorities responsible for validating vaccines, which has nevertheless made it possible to harmonize clinical trials as much as possible.
But they vary frankly all the same, and on several points.
The volunteer samples, to begin with, are obviously not the same.
"In the United States, for example, you will potentially have more comorbidities," comments Stéphane Paul, immunologist at the Saint-Étienne University Hospital and member of the Covid-19 vaccine scientific committee.
In Brazil or South Africa, you will have a younger population.
This can count in recruitments.
"
That's not all.
To calculate the number of contaminated volunteers, for example, the laboratories did not all choose the same time scale before counting the patients after vaccination.
Between Pfizer and Johnson & Johnson, the timeframe even varies from simple to quadruple (7 days for Pfizer, 28 for Johnson & Johnson).
Also, the trials were conducted in different countries.
When Moderna locates all of its sample in the United States, Pfizer is also exported to Brazil, Argentina and South Africa.
Johnson & Johnson has for its part also recruited in Peru and Chile.
“This is one of the variables that makes the comparison the most difficult,” points out Stéphane Paul.
This is even more true with the appearance of different variants, which are more contagious for some.
"
Coronavirus Newsletter
Update on the Covid-19 epidemic
Subscribe to the newsletterAll newsletters
Different countries ... But also different temporalities.
To understand the issue, let's first zoom in on the volunteers tested in the United States.
Moderna and Pfizer launched their trials almost simultaneously, in the height of summer, at the end of July.
The epidemic was then in the decline phase.
The clinical trial, as shown in the graph below, was therefore conducted there when the contaminations curve was at a low point.
Quite the opposite of Johnson & Johnson, which launched at the end of September when the terrible third wave was about to break.
If the comparison between the Placebo group and that of the vaccinated makes it possible to smooth these differences in temporality, the variants change the situation much more.
The Johnson & Johnson clinical trial was carried out in South Africa when the so-called “South African” variant hit the country.
Variant that is potentially more resistant to the vaccine than the original strain.
The Pfizer trial for its part ended just before the runaway on November 13, 2020.
Could labs be tempted to conduct their clinical trials when the epidemic situation is most favorable?
Asked about this, the Pfizer laboratory denies any calculation.
“The rate of circulation of the coronavirus was a criterion for selecting the countries where the clinical study was conducted, the company swears.
In August 2020 and in the months that followed, the coronavirus was actively circulating in a large number of countries, including the United States and Brazil.
The virus was circulating actively but still remained in a declining phase, verification made.
Stéphane Paul cannot really imagine the laboratories trying out these kinds of little games.
"When a trial is carried out in the epidemic phase, the number of contaminations increases more rapidly in the placebo group," observes the immunologist from the scientific committee.
The effectiveness of a vaccine can be judged more quickly.
But do not believe that laboratories prefer to bet on a period of calm to hope for more flattering results.
Instead, they prefer to go and test their vaccines where the epidemic strikes the most.
A vaccine works or it doesn't.
I would add that in the case of Covid, the laboratories simply did it as quickly as possible, launching their tests as soon as possible.
"
Health policies at the heart of the debate
The debate on the effectiveness of vaccines is also semantic.
What do we expect from the Covid-19 vaccines?
“It is also a question of health policy, analyzes Stéphane Paul.
If you prioritize a vaccine for its ability to reduce transmissions, then you plan to immunize children from the start, for example.
If, on the other hand, you prioritize reducing mortality, relieving hospitals and resuscitation services, then you are targeting the target population more.
“The majority of countries affected by the virus, faced with the emergency, opted for this second strategy.
And in terms of hospitalizations and deaths, the test results could not be more reassuring.
None of the volunteers who received doses of the vaccine died.
Better, none has been hospitalized.
Whether the vaccines are 95% or 66% “effective”.
This is why there is no point in trying to compare the efficacy rates of vaccines.
"This does not mean that these data are devoid of interest," continues the immunologist.
They make it possible to measure the effects of a vaccine over a given time and on a given population ”.
In other words, they must be treated in isolation.
The AstraZeneca case is also very interesting.
"The first data obtained in real life, in Scotland and Israel for example, show that the vaccine is very effective, even more than in the clinical trial."
A rather rare fact, which follows some hiccups observed during the clinical trial.
The numbers have been changed several times, outdated data has been exploited for the phase 3 trial, which is not allowed and has led to a correction of the efficacy in recent days.
Volunteers have also received reduced doses of the vaccine without being warned.
It remains to be seen how much these hiccups, added to the research carried out on the cases of thrombosis currently being examined by the authorities, could harm its distribution.
When contacted, the laboratory did not respond to our requests.